With the advent of potent antiretroviral therapies, the life expectancy of individuals with HIV has increased dramatically, and HIV clinical care has transitioned to a chronic disease model. In recent years, proportionately fewer individuals with HIV experience AIDS-related complications compared with non-AIDS serious illnesses, such as cardiovascular disease and non-AIDS-defining malignancies.[1] Consequently, clinicians who provide primary care to persons with HIV should have the knowledge and skills to recognize and manage common primary care conditions and to implement evidence-based prevention measures. This review will explore several common topics in the primary care management of persons with HIV.
- Module 2 Overview
Basic HIV Primary Care - 0%Lesson 1
Initial EvaluationActivities- 0%Lesson 2
Oral ManifestationsActivities- 2A.Core Concepts
- 2B.Implementing Oral Health Care into HIV Primary Care Settings Curriculum
- 2C.Intraoral Examination
- 2D.How to Check Patients for Oral Cancel
- 0%Lesson 3
Cutaneous ManifestationsActivities- 0%Lesson 4
Immunizations in AdultsActivities- 0%Lesson 5
Primary Care ManagementActivities- 0%Lesson 6
Screening for Mental Health ConditionsActivities- 0%Lesson 7
Substance Use DisordersActivities- 0%Lesson 8
Retention in HIV CareActivitiesLesson 5. Primary Care Management
Learning Objective Performance Indicators
- Discuss the evaluation of common comorbidities in people with HIV
- Explain appropriate management of common comorbidities in people with HIV
- Summarize key similarities and differences in managing medical comorbidities in people with and without HIV
- Discuss tobacco use and smoking cessation strategies in people with HIV
- List cancer screening recommendations for persons with HIV
Last Updated: August 26th, 2024Author:Jehan Z. Budak, MDJehan Z. Budak, MD
Assistant Professor of Medicine
Division of Allergy & Infectious Diseases
University of WashingtonDisclosures: NoneReviewer:David H. Spach, MDDavid H. Spach, MD
Professor of Medicine
Division of Allergy & Infectious Diseases
University of WashingtonDisclosures: NoneTable of ContentsTopic Overview
Cancer Screening
Overview
People with HIV have an overall increased risk of cancer (and younger age of onset) compared with the general population.[2,3,4] Research suggests a correlation between HIV-related immunodeficiency and malignancy, possibly through a mechanism of immune dysregulation and decreased immune surveillance; it is now well recognized that a low CD4 cell count increases the risk of malignancy.[5,6] As persons with HIV live longer in the current era of effective antiretroviral therapy, a shift has occurred from predominantly AIDS-defining malignancies to non-AIDS-defining malignancies.[6,7,8,9] Since 2003, the number of non-AIDS-defining malignancies has exceeded the number of AIDS-defining malignancies, and consequently, clinicians must be vigilant in surveillance for all forms of malignancy, AIDS-associated or not.
Changing Cancer Epidemiology in Persons with HIV
Data from the CDC and the HIV/AIDS Cancer Match Study showed a sharp increase in non-AIDS-defining cancers among persons with HIV from 1991 through 2005.[8,10] Additional data suggest the trend of increasing non-AIDS-defining cancers will continue and that by 2030, prostate and lung cancer will be the most common types of cancer in people with HIV.[4] Kaposi’s sarcoma and non-Hodgkin's lymphoma (both AIDS-defining malignancies), along with lung cancer (linked to excess tobacco exposure), are currently the most common cancers in persons with HIV.[4,11] In a recent study among individuals with HIV in the United States, half of all excess deaths were due to AIDS-defining cancers (Kaposi's sarcoma, non-Hodgkin’s lymphoma, and cervical cancer), and half were due to non-AIDS-defining cancers (lung, anal, liver, oral/pharyngeal cancers); most of these cancers are mediated by viral coinfections.[12] In this same study, there was no excess of colon, breast, or prostate cancer among persons with HIV compared with the general population.[12] Other studies have shown rates of prostate and colorectal cancer similar to or slightly lower than in the general population.[8,13]
Cancer Surveillance
The shifting spectrum of cancer in persons with HIV underscores the importance of incorporating standardized cancer surveillance practices in the care of persons with HIV, including those with relatively preserved immune function. The U.S. Preventive Services Task Force (USPSTF) USPSTF has recommendations for cancer screening, but these are for the general population and not specific to people with HIV. Recommendations regarding screening for malignancies specific to individuals with HIV have also been issued.
Cancer Screening Recommendations Not Impacted by HIV
Breast Cancer Screening
In the United States, breast cancer is the most common cancer in women, regardless of race or ethnicity.[14] Although unusual clinical presentations and more rapid progression of breast cancer have been reported among women with HIV, breast cancer prevalence does not appear to be increased in women with HIV.[15] The HIVMA/IDSA Primary Care Guidance recommends that women with HIV follow the same breast cancer screening guidelines as for women without HIV.[16] Nevertheless, there are some differences among professional organizations as to the optimal age of initiation and the frequency of breast cancer screening in women with and without HIV.
- USPSTF Recommendations for Breast Cancer Screening: The USPSTF recommends biennial (every other year) screening mammography for women aged 40 to 74 years of age.[17] These recommendations state there is insufficient evidence to recommend for or against breast cancer screening in women 75 years of age and older.[17]
- American Cancer Society: For women who have an average risk of breast cancer, the American Cancer Society (ACS) recommends annual mammography screening beginning at age 45 years.[18,19] Women 40 to 44 years of age should have the opportunity to begin annual screening.[18] At 55 years of age, women should transition to biannual mammography screening or have the opportunity to begin annual mammography screening.[18] The ACS guidelines recommend that screening mammography should continue in women who have overall good health and a life expectancy of at least 10 years.[18]
Colon Cancer Screening
In the general United States population, colon cancer is the fourth most common cancer, accounting for approximately 50,000 deaths per year.[14,20] Although persons with HIV may have a slightly higher risk of developing colon cancer, screening for colon cancer in persons with HIV should not be based on HIV RNA levels or CD4 cell count. The HIVMA/IDSA Primary Care Guidance recommends that persons with HIV follow the same colon cancer screening recommendations as for persons without HIV.[16]
- USPSTF Recommendations for Colorectal Cancer Screening: The USPSTF recommends screening for colorectal cancer in adults between the ages of 45 and 75 years.[21] Decisions regarding colorectal cancer screening for persons aged 76 to 85 years should be individualized.[21] The USPSTF does not recommend performing routine screening in adults older than 85 years of age.[21] The USPSTF guidelines provide the following screening options, with the ultimate goal of improving screening rates: (1) stool-based tests (e.g., high sensitivity fecal occult blood testing [FOBT]), (2) fecal immunochemical testing (FIT), FIT-DNA testing, and (3) direct visualization tests (e.g. flexible sigmoidoscopy with or without FIT, colonoscopy, and computed tomographic colonography).[21] The screening interval depends on the screening modality and the results of the screening tests.
- American Cancer Society: In 2018, the American Cancer Society issued a guideline update, which recommends screening adults with an average risk of colorectal cancer starting at age 45 years.[22] This is a qualified recommendation (one in which there is clear evidence of benefit but less certainty about the balance of benefits and harms), whereas their recommendation to screen adults aged 50 years and older is a strong recommendation.[22]
- U.S. Multi-Society Task Force (USMSTF): In 2022, the USMSTF on Colorectal Cancer issued recommendations for colorectal cancer screening in the general population.[23] These guidelines recommend initiating screening at 45 years of age in persons at average risk.[23] The 2017 USMSTF guideline ranks the existing colon cancer screening tools as shown in the table below.[24] Table 1. U.S. Multi-Society Task Force on Colorectal Cancer
Multi-Society Task Force Ranking of Current Colorectal Cancer Screening Tests
Tier 1
- Colonoscopy every 10 years
- Annual fecal immunochemical test (FIT)
Tier 2
- CT colonography every 5 years
- FIT-fecal DNA every 3 years
- Flexible sigmoidoscopy every 10 years (or every 5 years)
Tier 3 - Capsule colonoscopy every 5 years
Available Tests Not Currently Recommended
- Septin 9
Source:- Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307-23. [PubMed Abstract]
- Post-Colonoscopy Follow-Up recommendations: In 2012, the USMSTF published updated recommendations for colonoscopy surveillance based on the most advanced findings from the baseline colonoscopy; these recommendations are summarized in the table below.[25,26] Table 2. U.S. Multi-Society Task Force on Colorectal Cancer
US Multi-Society Task Force Recommendations for Post-Colonoscopy Follow-Up in Average-Risk Adults With Normal Colonoscopy or Adenomasa
Baseline Colonoscopy:
Most Advanced Finding(s)Recommended Surveillance Interval Strength of Recommendation Quality of Evidence Normal 10 yearsb Strong High 1–2 tubular adenomas <10 mm 7-10 yearsc Strong Moderate 3-4 tubular adenomas <10 mm 3-5 years Weak Very low 5–10 tubular adenomas <10 mm 3 years Strong Moderate Adenoma >10 mm 3 years Strong High Adenoma with tubulovillous or villous histology 3 yearsd Strong Moderate Adenoma with high-grade dysplasia 3 yearsd Strong Moderate >10 adenomas on single examinatione 1 year Weak Very low Piecemeal resection of adenoma ≥20 mm 6 months Strong Moderatef aAll recommendations assume examination complete to cecum with bowel preparation adequate to detect lesions >5 mm in size; recommendations do not apply to individuals with a hereditary CRC syndrome, personal history of inflammatory bowel disease, personal history of hereditary cancer syndrome, serrated polyposis syndrome, malignant polyp, personal history of CRC, or family history of CRC, and must be judiciously applied to such individuals, favoring the shortest indicated interval based on either history or polyp findings.
bFollow-up may be with colonoscopy or other screening modality for average-risk individuals.
c Patients with recommendations issued before 2020 for shorter than 7- to 10-year follow-up after diagnosis of 1–2 tubular adenomas may follow original recommendations. If feasible, physicians may re-evaluate patients previously recommended an interval shorter than 10 y and reasonably choose to provide an updated recommendation for 7- to 10-year follow-up, taking into account factors such as quality of baseline examination, polyp history, and patient preferences.
dAssumes high confidence of complete resection.
ePatients with >10 adenomas or lifetime >10 cumulative adenomas may need to be considered for genetic testing based on absolute/cumulative adenoma number, patient age, and other factors such as family history of CRC (see text).
fSee US Multi-Society Task Force recommendations for endoscopic removal of colorectal lesions.
Source:- Gupta S, Lieberman D, Anderson JC, et al. Recommendations for Follow-Up After Colonoscopy and Polypectomy: A Consensus Update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2020;158:1131-53.e5. [PubMed Abstract]
Lung Cancer Screening
In the United States, lung cancer is the third most common cancer in men and women and the leading overall cause of cancer deaths.[14] Increasing age and cumulative exposure to tobacco smoke are cited as the two most important risk factors for lung cancer.[27,28] In persons with HIV, lung cancer is the leading cause of mortality from cancer.[29] Compared to the general population, persons with HIV have higher rates of lung cancer and may have poorer outcomes.[29] The National Lung Screening Trial is a large, multicenter, randomized, controlled trial that randomized participants aged 55 to 74 years at high risk for lung cancer to three annual screenings with either low-dose computed tomography or single-view posteroanterior chest radiography; screening with computed tomography offered a relative reduction in mortality from lung cancer of 20% compared to only 6.4% with chest radiography.[30] In a subsequent analysis of the National Lung Screening Trial with additional follow-up, investigators reported a relative risk reduction of 16%.[31] At this time, recommendations for lung cancer screening for people with HIV are the same as in the general population and are summarized by the following guidance.
- USPSTF Recommendations for Lung Cancer Screening: The USPSTF recommends annual screening with low-dose computed tomography in patients aged 50 to 80 years who have a greater than or equal to 20 pack-year smoking history if they are currently smoking or have quit smoking within the past 15 years.[28] Yearly screening should be discontinued if: (1) the person has not smoked for 15 years, or (2) they develop a health problem that limits their life expectancy or their ability or willingness to take part in curative strategies.
Prostate Cancer Screening
Men with and without HIV have a similar risk of prostate cancer.[2,11,13,32] The reduction in prostate cancer mortality achieved with prostate-specific antigen (PSA)-based screening is small, whereas the potential for patients to experience adverse effects from over diagnosis and unnecessary treatment is high. The HIVMA/IDSA Primary Care Guidance recommends similar screening for prostate cancer in persons with HIV as for those without HIV.[16]
- USPSTF Recommendations for Prostate Cancer Screening: The USPSTF recommends prostate cancer screening should be an individualized decision for men 55 to 69 years of age.[33] The guidelines note that the three most important risk factors for prostate cancer are: older age, African American race, and family history.[33] The recommended screening test, if performed, is a measurement of the level of prostate-specific antigen (PSA) in the blood.[33] For men 70 years of age and older, the USPSTF guidelines recommend against routine screening for prostate cancer.[33] The USPSTF recommends that prostate cancer screening in transgender persons should be based on the presence or absence of a prostate, not on the person's identified gender.[33]
Cancer Screening Recommendations Specific to HIV
Cervical Cancer Screening
Abnormal cervical cytology is nearly 11 times more common among cisgender persons with HIV compared with individuals without HIV. Cervical cancer screening recommendations differ slightly between persons with HIV and those without HIV, as outlined below and in the Adult and Adolescent OI Guidelines.[34] The main difference is that cervical cancer screening for persons with HIV tends to start at an earlier age, occurs with more frequency, and continues for longer than in persons without HIV.[34] The following recommendations refer to all people with HIV who have a cervix, including persons who identify as cisgender women, transgender men, and gender nonbinary individuals.[34]
- Age of Onset for Cervical Cancer Screening: Initiation of cervical cancer screening is recommended beginning at 21 years of age.
- Duration of Cervical Cancer Screening: Cervical cancer screening should continue throughout their life, as opposed to the recommendation in the general population to stop cervical cancer screening after 65 years of age.
- Cervical Cancer Screening at Entry to HIV Care: Persons with HIV who are sexually active and at least 21 years of age should undergo cervical cancer screening at initial entry to HIV care and again 12 months later. The screening test used should be determined by the person’s age, as reviewed below.
- Cervical Cancer Screening if 21-29 Years of Age: Annual cervical Papanicolaou (Pap) testing is recommended in people with HIV who are 21-29 years of age, but if 3 consecutive annual screens are normal, cervical Pap tests can be performed every 3 years. Co-testing with HPV is not recommended for routine screening in this age group due to a high HPV prevalence, but HPV testing can be done reflexively on abnormal cervical Pap results to direct further evaluation.
- Cervical Cancer Screening if 30 Years of Age or Older: People with HIV who are 30 years of age and older should have either (1) cervical cancer screening by Pap testing alone or (2) Pap testing plus simultaneous HPV co-testing. Most experts prefer the second option if available. If Pap testing alone is used, it should be performed at baseline and every 12 months; if the results of 3 consecutive Pap tests are normal, then follow-up testing can occur every 3 years. If Pap and HPV co-testing is performed and both are negative, follow-up screening can be performed in 3 years.
- Summary of Cervical Cancer Screening Algorithms for Persons with HIV: The figure below summarizes guidelines for managing normal and abnormal cervical cytology results in persons with HIV who are 21-29 years of age and in those 30 years of age and older; for persons 30 years of age and older, the recommendations differ based on whether high-risk human papillomavirus (hr-HPV) testing is performed (Figure 1). Note that cervical cancer screening recommendations are not altered in persons who have received prior HPV vaccination.
Anal Cancer Screening
Anal cancer risk is higher in people with HIV compared to people without HIV. The incidence of anal cancer in men with HIV who have sex with men is particularly high, estimated to be 89 per 100,000 person-years, which is about 55 times higher than the incidence in the general adult population (1.6 per 100,000 person-years) and 4 to 5 times higher than the incidence among women with HIV (19 per 100,000 person-years).[2,11,35,36] Infection with HPV has been implicated in the pathogenesis of most anal malignancies. Anal dysplasia refers to precancerous lesions, including low-grade squamous intraepithelial lesions (LSIL) and high-grade squamous intraepithelial lesions (HSIL). The ANCHOR study is a national randomized clinical trial to determine if the treatment of biopsy-proven anal HSIL reduces the incidence of anal cancer in persons with HIV.[37] Results showed that the rate of progression to anal cancer was 57% lower in the treatment group, as compared to the active monitoring group.[37] Previously there were no formal recommendations for anal cancer screening in persons with HIV, but following results from the ANCHOR study, new guidance for anal cancer screening in people with HIV was issued in the Adult and Adolescent OI Guidelines on July 9, 2024; these recommendations are summarized below.[34]
- General Approach to Anal Cancer Screening: Based on the high incidence of anal cancer in persons with HIV, the high prevalence of anal HSIL in persons with HIV, high rates of progression of anal HSIL to anal cancer in the absence of treatment, and the efficacy in treating anal HSIL to reduce progression to anal cancer, it is recommended to screen for anal cancer and treat anal HSIL if found. The approach to anal cancer screening is highly dependent on whether clinics have access to high resolution anoscopy (HRA).
- Age to Initiate Screening: When to start screening for anal cancer in asymptomatic individuals with HIV should be based on the overall risk for anal cancer and begins at different ages depending on sex and HIV risk group.[34,36] Based on the incidence of anal cancer risk, screening for anal precancer and cancer is recommended to begin at 35 years of age for MSM and transgender women who have HIV and to begin at 45 years of age for all others with HIV. For MSM and transgender persons with HIV younger than 35 years of age and all others with HIV younger than age 45 years, anal symptoms should be evaluated with digital anorectal exam (DARE) and standard anoscopy.
- Screening Modalities: There are multiple modalities that can be utilized for routine anal cancer screening, including symptom screening, DARE, standard anoscopy, anal cytology, and hr-HPV, co-testing. The decision of whether to use anal cytology in routine screening depends on whether HRA is available for evaluation of abnormal screening cytology tests.
- Symptom Screen: At a minimum, every person with HIV, regardless of history of anal intercourse, should undergo an annual assessment of anal symptoms (e.g., ask about unexplained itching, anal bleeding, anal pain, and presence of anal or perianal lesions).
- Screening when HRA is Not Available: If access to HRA is not available, the recommendation is to assess anal symptoms and perform DARE. Although somewhat dependent on clinician experience, DARE can potentially detect masses associated with anal neoplasm or dysplasia, anal warts, anal discharge that may indicate a sexually transmitted infection, and prostate abnormalities. When HRA is not available, the presence of anal symptoms or an abnormal DARE should be followed by a standard anoscopy examination.
- Screening when HRA is Available: If HRA is available, the recommendation is to assess anal symptoms, collect anal cytology specimens, and perform DARE (after collection of the cytology specimen). Screening of anal specimens can occur using anal cytology alone or with high-risk HPV co-testing, which tests for HPV types 16 and 18. The presence of anal symptoms or an abnormal DARE should result in HRA.
- Management of Abnormal Anal Cytology Test Result: Management of an abnormal anal cytology result (ASC-US or worse) depends on the level of the abnormality on anal cytology and whether hr-HPV co-testing was used.
- Regardless of hr-HPV co-testing, the presence of LSIL or HSIL should result in HRA.
- If hr-HPV co-testing was not performed, and cytology results have ASC-US or worse, HRA is needed.
- If hr-HPV co-testing was performed, and cytology results have ASC-US, management of this result depends on the results of the hr-HPV co-test. If hr-HPV co-testing was performed, and cytology results have LSIL or HSIL, then HRA is needed.
- Summary of Anal Cancer Screening Algorithms for Persons with HIV: The figure below summarizes the Adult and Adolescent OI Guidelines guidelines for anal cancer screening in people with HIV, including assessment of anal cytology and hr-HPV (Figure 2).[34] When anal cytology is implemented in a clinical setting, it is critical to establish a follow-up plan and to ensure access to providers who can deliver these follow-up services.
Cardiovascular
Cardiovascular Risk
There are many factors that influence and increase cardiovascular disease risk, including hypertension, hyperlipidemia, diabetes mellitus, and smoking. These factors are addressed separately in this Topic Review. This section will briefly address cardiovascular risk and include a discussion of aspirin prevention for cardiovascular disease (CVD) prevention and screening for abdominal aortic aneurysm. Statin use for primary prevention of CVD is discussed below in the Hyperlipidemia section.
Aspirin for Cardiovascular Disease Prevention
For persons with a documented history of CVD, aspirin for secondary prevention is strongly recommended. In contrast, the use of aspirin as primary prevention (i.e., for those in whom CVD has not yet been diagnosed) remains controversial. More recently, three large randomized controlled trials involving different populations (HIV was not an exclusion) examined the impact of aspirin 100 mg daily for primary prevention of CVD.[38,39,40] In all three studies, the risk of bleeding outweighed the benefit of preventing CVD (Figure 3).[41] The following summarizes professional guideline recommendations regarding aspirin use for primary prevention.
- USPSTF: In 2022, the USPSTF recommended against initiation of low-dose aspirin as primary prevention in adults 60 years or older.[42] The USPSTF also recommended that in adults 40 to 59 years with a 10-year Atherosclerotic Cardiovascular Disease (ASCVD) risk of 10% or greater, the decision to initiate low-dose aspirin for primary prevention of CVD should be individualized.[42]
- ACC/AHA: The American College of Cardiology/American Heart Association (ACC/AHA) recommends considering aspirin for select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk.[43,44]
- ADA: The American Diabetes Association (ADA) states aspirin may be considered as primary prevention in those with diabetes who are at increased CVD risk after a discussion regarding benefits versus the increased risk of bleeding.[45]
Screening for Abdominal Aortic Aneurysm (AAA)
An abdominal aortic aneurysm (AAA) is defined by the abnormal dilation of the abdominal aorta to a maximum diameter of 3 cm or greater.[46] Most AAAs are asymptomatic until they rupture, and when that occurs, the mortality rate is high. The prevalence of AAA is generally greater in older individuals, particularly men, but the most important risk factor for AAA is smoking.[47] Thus, the USPSTF recommends one-time AAA screening with ultrasonography for men 65 to 75 years of age who have ever smoked.[48]Special Considerations in Persons with HIV
Cardiovascular Risk in Persons with HIV
Cardiovascular and cerebrovascular disease are of special importance for individuals with HIV, with evidence showing a 1.5- to 2-fold greater risk of CVD in people with HIV when compared with those without HIV.[49,50] The increased CVD risk conferred by HIV has now been demonstrated in the Global Burden of Atherosclerotic Cardiovascular Disease in People Living with HIV, the Kaiser Observational Study and the Veterans Aging Cohort Study (Figure 4).[49,51,52] Rates of heart failure, stroke, pulmonary hypertension, and sudden cardiac death are also higher for people with HIV, even those taking antiretroviral therapy with suppressed HIV RNA levels.[53] For these reasons, many experts consider HIV an independent CVD risk factor, especially in persons with HIV and more advanced immunosuppression.
Factors Associated with Increased Cardiovascular Risk in Persons with HIV
The increased risk of CVD in persons with HIV is potentially mediated by (1) traditional risk factors, such as dyslipidemia, obesity, and cigarette smoking, (2) metabolic alterations related to antiretroviral therapy (e.g., insulin resistance and dyslipidemia), and (3) factors linked to HIV itself, including immune activation and inflammation.[50,53,54] In addition, CVD in persons with HIV disproportionately affects Hispanic and Black individuals.[55,56,57]
Cardiovascular Risk and Antiretroviral Therapy
The overall benefits of antiretroviral therapy clearly outweigh the risks. In the Strategies for Management of Antiretroviral Therapy (SMART) trial, continuous antiretroviral therapy compared to intermittent (driven by CD4 count) antiretroviral therapy decreased all-cause mortality, including death from cardiovascular disease.[58] Nevertheless, studies examining individual drug and class effects have raised concerns regarding the contribution of abacavir and protease inhibitors (PIs) to cardiovascular risk, although results have been conflicting.[49,59,60,61,62] The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study found that recent abacavir use conferred the highest relative rate of myocardial infarction (relative rate of 1.89, even after controlling for traditional cardiovascular risk factors); in the D:A:D study, the abacavir effect appeared to be reversible after the drug was stopped.[63,64,65] Based on existing data, most experts would avoid abacavir in those with CVD.
Cardiovascular Risk Reduction Strategies in Persons with HIV
Cardiovascular risk reduction in persons with HIV is multifactorial, but general measures based on the available literature include the following:[53,66,67]
- Start antiretroviral therapy as soon as possible after diagnosis
- Achieve and sustain suppressed HIV RNA levels
- Encourage smoking cessation
- Promote physical activity
- Manage lipid, blood pressure, and glycemic abnormalities
- Avoid heavy alcohol use
- Adhere to American College of Cardiology (ACC)/American Heart Association (AHA) dietary guidelines
Aspirin for Cardiovascular Disease Prevention in Persons with HIV
Studies evaluating aspirin as primary prevention of CVD in people with HIV have not been done. Ultimately, the AHA Scientific Statement on “Characteristics, Prevention, and Management of CVD in People Living with HIV” recommends that “further studies are needed to elucidate the role of antithrombotic therapy for ASCVD prevention in HIV.”[53]
Screening for Abdominal Aortic aneurysm (AAA) in Persons with HIV
The AAA screening recommendations are the same for persons with HIV as for those without HIV—a one-time screening with ultrasonography for men 65 to 75 years of age who have ever smoked.[48] The overall risk of AAA among people with or without HIV is approximately the same, but the risk of AAA is higher in persons with HIV if they have a CD4 cell count of less than 200 cells/mm3 or an HIV-1 RNA level greater than 500 copies/mL.[68]Diabetes Mellitus
Overview
Diabetes mellitus affects approximately 11% of the United States population aged 20 years and older and contributes to significant morbidity, decreased quality of life, rising health care costs, and mortality.[69] Patients with diabetes mellitus require frequent monitoring of laboratory values and the development of microvascular complications, including kidney disease, retinopathy, neuropathy, and atherosclerotic cardiovascular disease. The following discussion will focus primarily on type-2 diabetes mellitus.
Current Guidelines
The American Diabetic Association (ADA) maintains updated guidelines pertaining to the screening, diagnosis and management of diabetes, with the most recent version published in 2023.[45,70,71,72,73,74,75,76,77,78,79...] Recommendations in the most recent version of these guidelines are outlined below.
Diabetes-Specific Recommendations
- Indications for Diabetes Screening: Routine screening for type 2 diabetes mellitus and prediabetes should be considered in all adults who are overweight or obese (BMI 25 kg/m2 or greater) and have at least one additional risk factor for diabetes, such as physical inactivity or a first-degree relative with diabetes.[75] In the absence of additional risk factors, overweight and obese adults should be screened starting at age 35 years.[75] If tests are normal, screening should be repeated approximately every 3 years.[75] Table 3. American Diabetes Association (ADA) Standards of Medical Care in Diabetes—2023
Criteria for Testing for Diabetes or Prediabetes in Asymptomatic Adults
1. Testing should be considered in overweight or obese (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian Americans) adults who have one or more of the following risk factors:
- First-degree relative with diabetes
- Race/ethnicity with increased risk of developing diabetes (e.g., African American, Latino, Native American, Asian American, Pacific Islander)
- History of cardiovascular disease
- Hypertension (≥130/80 mmHg or on therapy for hypertension)
- HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L)
- Women with polycystic ovary syndrome
- Physical inactivity
- Other clinical conditions associated with insulin resistance (e.g., severe obesity, acanthosis nigricans)
2. Patients with prediabetes (HbA1c ≥5.7% [39 mmol/mol], impaired glucose tolerance, or impaired fasting glucose) should be tested yearly. 3. Women who were diagnosed with gestational diabetes mellitus should have lifelong testing at least every 3 years. 4. For all other patients, testing should begin at 35 years of age. 5. If results are normal, testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status. 6. People with HIV Source:- ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S19-S40. [PubMed Abstract]
- Diabetes Diagnostic Criteria: The diagnosis of diabetes mellitus can be made using the following criteria:
- Fasting plasma glucose greater than or equal to 126 mg/dL (fasting defined as no caloric intake for 8 or more hours), or
- 2-hour plasma glucose greater than or equal to 200 mg/dL during an oral glucose tolerance test using the equivalent of a 75-gram glucose load, or
- HbA1c greater than or equal to 6.5%, or
- A random glucose greater than or equal to 200 mg/dL in a patient with classic symptoms of hyperglycemia or with hyperglycemia crisis.
- Definition of Prediabetes: Individuals are defined as having prediabetes if screening tests reveal any one of the following: (1) fasting glucose of 100 to 125 mg/dL, (2) a 2-hour plasma glucose level of 140 to 199 mg/dL after an oral glucose tolerance test, or (3) HbA1c of 5.7 to 6.4%.[75] Individuals with prediabetes should be informed of their increased risk of developing type 2 diabetes and cardiovascular disease, and they should be encouraged to pursue lifestyle modifications, including weight loss and increased physical activity, to lower these risks.[75] Repeat screening should occur annually in this population.
- Pharmacologic Therapy: For persons who meet the criteria for type 2 diabetes, pharmacologic therapy, in addition to lifestyle modifications, is warranted.[71] Metformin is the preferred initial pharmacologic agent in the treatment of type 2 diabetes mellitus as long as it is not contraindicated and the patient can tolerate it.[71] For persons with diabetes in whom atherosclerotic heart disease, heart failure, or chronic kidney disease predominates, the treatment regimen should include an agent that decreases cardiorenal risk, such as a GLP-1 receptor agonist or a sodium-glucose cotransporter 2 (SGLT2) inhibitor that has demonstrated cardiovascular risk reduction.[71] Some individuals with diabetes will require additional oral hypoglycemic agents or insulin in addition to the agents listed above.[71] Treatment should be individualized and patient-centered when adding a second agent to metformin.
- Monitoring and Goal for HbA1c: Ongoing monitoring of HbA1c is recommended every 6 months if at treatment goal or every 3 months if not at goal or if therapy has changed.[73] The ideal HbA1c target is unclear, but recommended targets range from the most stringent goal of less than 6.5% to the least stringent goal of less than 8.0%.[73] Targeting stringent control is controversial given the finding from a large randomized control trial (ADVANCE) that found no evidence that maintaining an HbA1c of less than 6.5% provided long-term benefit with respect to mortality or macrovascular events.[80] A goal HbA1c of less than 7.0% is considered an appropriate goal for many nonpregnant adults.[73] A less stringent goal (HbA1c less than 8.0%) is considered appropriate for some individuals with diabetes, especially if they have experienced severe hypoglycemia, or other factors are present, such as a short life expectancy or existing major complications from long-standing diabetes.[73]
Screening and Management of Complications
- Screening for Complications: Persons should undergo annual screening for complications of type 2 diabetes, including nephropathy, retinopathy, and neuropathy.[70] Annual screening for chronic kidney disease should consist of urinary albumin (e.g., spot urinary albumin-to-creatinine ratio) and estimated glomerular filtration rate in persons with type 1 diabetes with a duration of 5 years or longer and those with type 2 diabetes.[70] Comprehensive and dilated eye examinations and determination for follow-up should be conducted by an ophthalmologist or an optometrist.[70] Persons with type 2 diabetes should be assessed for diabetic peripheral neuropathy starting at diagnosis, and those with type 1 should undergo assessment 5 years after the diagnosis; thereafter, screening for neuropathy should occur at least annually. Screening for neuropathy should also include screening for distal symmetric polyneuropathy and autonomic neuropathy.[70]
- Lifestyle Management: Persons with diabetes should receive individualized counseling for nutritional therapy, psychosocial support, smoking cessation (if indicated), and self-management support.[78] Exercise guidelines recommend, in general, at least 150 minutes per week of moderate-intensity aerobic activity and at least twice-weekly resistance training.[78]
- Use of Aspirin in Persons with Diabetes: Those with diabetes and a history of ASCVD should receive a daily low-dose aspirin (75 to 162 mg) as a secondary prevention strategy.[45] Daily low-dose aspirin may be considered for use as a primary cardiovascular disease prevention strategy for individuals with diabetes who have increased cardiovascular risk, but this should be a shared decision-making process weighing the benefits versus the risk of bleeding.[45] In the ASCEND Trial, which included individuals with diabetes, the risk of bleeding still outweighed the benefit of preventing CVD.[38]
- Treatment of Hypertension in Persons with Diabetes: For individuals with diabetes and hypertension, the ADA recommends a target blood pressure of less than 130/80 mmHg.[45] This can be achieved with either an angiotensin-converting enzyme (ACE) inhibitor, angiotensin II blocker (ARB), thiazide-type diuretic, or calcium channel blocker. For those with microalbuminuria, an ACE or ARB should be the first-line choice.[45]
- Lipid Screening and Management of Hyperlipidemia: Lipid screening is advised in adults with type 2 diabetes at baseline and at least every 5 years thereafter.[45] For persons with diabetes who require treatment for lipid disorders, a lipid profile should be obtained at initiation of lipid-lowering therapy, within 4 to 12 weeks after initiating or changing therapy, and yearly thereafter.[45] Increased LDL should be managed aggressively with statin therapy and in accordance with the 2018 ACC/AHA Cholesterol Treatment Guidelines.[45,81]
Special Considerations for Persons with HIV
Screening for Diabetes
In the modern era of HIV treatment, the prevalence of diabetes mellitus in persons with HIV is estimated at 2 to 14%.[82] The HIVMA/IDSA Primary Care Guidance recommendations for the evaluation of diabetes in persons with HIV are as follows:[16]
- Screening for Diabetes in Persons Not on Antiretroviral Therapy: The HIVMA/IDSA HIV Primary Care Guidance recommends that prior to starting antiretroviral therapy, all persons with HIV should have screening for diabetes with a blood glucose (random or fasting) level and HbA1c.[16] If a random blood glucose value is greater than 200 mg/dL then a fasting blood glucose should be obtained. For persons not taking antiretroviral therapy, the diagnosis of diabetes is established with the same criteria as for persons without HIV. The ADA Guidelines recommend screening for diabetes with a fasting glucose test before starting antiretroviral therapy.[75]
- Screening for Diabetes in Persons Taking Antiretroviral Therapy: For persons taking antiretroviral therapy, only evaluation of plasma glucose (random or fasting) should be used for diabetes screening.[16] The use of HbA1c is not recommended for diagnosing diabetes in persons with HIV who are taking antiretroviral therapy, primarily because HBA1c may underestimate glycemia in this setting.[75] The ADA Guidelines recommend screening for diabetes at the time of switching antiretroviral therapy and 3 to 6 months after starting or switching antiretroviral therapy.[75] Subsequently, repeat screening for diabetes in persons taking antiretroviral therapy should be performed annually.
General Approach to Management of Diabetes in Persons with HIV
In general, the management of diabetes in persons with HIV should occur according to the ADA guidelines.[71,72,73]
- Management of Diabetes in Persons with HIV: In most cases, persons with HIV and mild blood glucose abnormalities can be effectively managed with lifestyle changes that include weight loss, increased exercise, and dietary modification.[72,78] If therapeutic intervention is warranted, initiating treatment with metformin is preferred.[71]
- Monitoring Glycemic Status: Individuals with HIV who have diabetes should have glycemic status (HbA1c or other glycemic measurement) monitored at least twice a year, with quarterly monitoring recommended with therapy changes and when glycemic goals are not met.[73] The glycemic goal for nonpregnant adults is an HBA1c of less than 7% without significant hypoglycemia; the blood glucose target goal is to have greater than 70% of readings in the target range of 70-180 mg/dL.[73]
- Screening for Renal Disease: In addition to routine monitoring of kidney function (addressed in the section on chronic kidney disease), persons with HIV should have annual monitoring of urine albuminuria in accordance with the ADA guidelines.[74,83]
- Antiretroviral Therapy: In most individuals, switching the antiretroviral regimen is not beneficial for impaired glucose tolerance. It is, however, important to evaluate potential drug interactions as some antiretroviral medications can indirectly contribute to elevated plasma glucose levels. For example, protease inhibitors and cobicistat can increase drug levels of quetiapine or certain corticosteroids (inhaled or oral) and thus cause hyperglycemia. In addition, for individuals who start antiretroviral therapy and have substantial weight gain associated with hyperglycemia, consideration should be given to a regimen to switch if the weight gain is likely attributed to the antiretroviral regimen.
- Use of Metformin and Antiretroviral Medications: The use of metformin with certain antiretroviral medications should also be carefully monitored. For example, concurrent use of metformin with dolutegravir or bictegravir can increase the concentrations of metformin.[84]
Hypertension
Overview
Hypertension is the most common diagnosis seen in primary care, and untreated hypertension increases the risk of myocardial infarction, stroke, renal failure, and death. According to the National Health and Nutrition Examination Survey (NHANES), from 2017 through 2018, the age-adjusted prevalence of hypertension among persons aged 18 years and older was 45.4% (Figure 5).[85]
Definition of Hypertension
The 2017 ACC/AHA Hypertension Guideline revised the definition of hypertension as any systolic blood pressure of at least 130 mm Hg or any diastolic BP of at least 80 mm Hg (Figure 6).[86]
Baseline Evaluation of Persons with Hypertension
The initial evaluation of patients with hypertension has three primary objectives: (1) to assess lifestyle and other risk factors that may affect prognosis and guide treatment of hypertension, (2) to reveal identifiable secondary causes of hypertension (such as renovascular or thyroid disease), and (3) to identify the presence or absence of target-organ damage and cardiovascular disease.[86] The 2017 ACC/AHA Hypertension Guideline recommends a baseline evaluation for all persons with hypertension that should include an electrocardiogram, complete blood count, sodium, potassium, creatinine with estimated glomerular filtration rate, calcium, thyroid stimulating hormone, urinalysis, a lipid profile, and fasting blood glucose.[86]
Current Guidelines for the Management of Hypertension
The 2017 ACC/AHA Hypertension Guideline addresses thresholds for treatment initiation, blood pressure goals, and recommendations regarding medication treatment.[86] The key points from these guidelines are summarized below:[86]
- For adults with hypertension, the recommended blood pressure treatment goal is less than 130/80 mm Hg. Some experts suggest an individualized and higher blood pressure target in the context of frailty, independence, and tolerability of treatment.[87]
- For persons with stage 1 hypertension, the American College of Cardiology ASCVD Risk Estimator should be used to determine the estimated 10-year risk for heart disease and stroke. If the risk is less than 10%, start with healthy lifestyle recommendations and reassess in 3 to 6 months; pharmacologic therapy is recommended when the risk is greater than 10%.
- Lifestyle modification is the foundation for cardiovascular risk reduction, and counseling should be provided to all persons with hypertension and continued throughout the management of the disease. The following are recommended lifestyle changes: (1) use the Dietary Approach to Stop Hypertension (DASH), (2) lose excess body weight, (3) reduce dietary intake of sodium, (4) increase dietary intake of potassium, (5) incorporate a weekly routine of physical activity that includes aerobic exercise, dynamic resistance training, and isometric resistance training, and (6) reduce consumption of alcohol.
- First-line initial pharmacotherapy for stage 1 hypertension, when indicated, should consist of treatment with a thiazide-type diuretic, calcium-channel blocker, angiotensin-converting-enzyme inhibitor, or angiotensin-receptor blocker; a repeat evaluation of blood pressure should occur in 1 month. This strategy should be used with caution in older individuals.
- Initial pharmacotherapy for stage 2 hypertension should consist of simultaneous administration of two agents of different classes (thiazide-type diuretic, calcium-channel blocker, angiotensin-converting-enzyme inhibitor, or angiotensin-receptor blocker). This strategy should be used with caution in older individuals.
- Avoid the simultaneous administration of an angiotensin-converting-enzyme inhibitor and an angiotensin-receptor blocker.
- For Black individuals with hypertension who do not have heart failure or chronic kidney disease, the preferred initial therapy is either a thiazide-type diuretic or a calcium-channel blocker.
- For all individuals with chronic kidney disease (stage 3 or higher, or stage 1 or 2 with albuminuria [≥300 mg/day, or ≥300 mg/g albumin-to-creatinine ratio in the first morning void]), the antihypertensive regimen should include an angiotensin-converting-enzyme inhibitor, or an angiotensin-receptor blocker if the angiotensin-converting-enzyme inhibitor is not tolerated.
Table 4. 2017 Hypertension Guidelines: Blood Pressure Targets and Treatment Recommendations
BP Category Systolic Diastolic Treatment or Follow-Up Normal <120 mm/Hg and <80 mm/Hg Evaluate yearly; encourage healthy lifestyle changes to maintain normal BP Elevated 120-129 mm/Hg and <80 mm/Hg Recommend healthy lifestyle changes and reassess in 3 to 6 months Hypertension: Stage 1 130-139 mm/Hg or 80-89 mm/Hg Assess the 10-year risk for heart disease and stroke using the atherosclerotic cardiovascular disease (ASCVD) risk calculator
- If risk is less than 10%, start with healthy lifestyle recommendations and reassess in 3 to 6 months
- If risk is greater than 10% or the patient has known clinical cardiovascular disease (CVD), diabetes mellitus, or chronic kidney disease, recommend lifestyle changes and BP-lowering medication (1 medication); reassess in 1 month for effectiveness of medication therapy
- If goal is met after 1 month, reassess in 3 to 6 months
- If goal is not met after 1 month, consider different medication or titration
- Continue monthly follow-up until control is achieved
Hypertension: Stage 2 ≥140 mm/Hg or ≥90 mm/Hg Recommend healthy lifestyle changes and BP-lowering medication (initiate with 2 medications of different classes); reassess in 1 month for effectiveness
- If goal is met after 1 month, reassess in 3 to 6 months
- If goal is not met after 1 month, consider different medications or titration
- Continue monthly follow-up until control is achieved
Source:- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269. [PubMed Abstract]
Special Considerations for Persons with HIV
Hypertension in Persons with HIV
Hypertension is common in people with HIV, and it increases the risk of acute myocardial infarction.[88,89,90] In people with HIV, the presence of hypertension is associated with traditional risk factors such as increasing age, obesity, African American race, diabetes, or hyperlipidemia.[90]
Management of Hypertension in People with HIV
Management of hypertension in people with HIV is not specifically addressed by the 2017 ACC/AHA Hypertension Guideline referenced above or by the HIVMA/IDSA Primary Care Guidance.[16,86] Nevertheless, since both hypertension and HIV are cardiovascular risk factors, both should be managed aggressively, and it is reasonable to follow the recommendations in the 2017 ACC/AHA Hypertension Guideline.[86] In addition, clinicians should consider the risk of drug interactions when adding any antihypertensive medication to a background of antiretroviral therapy. In particular, clinicians should use caution when administering calcium channel blockers, such as amlodipine, diltiazem, felodipine, nifedipine, and verapamil, in patients taking protease inhibitors or cobicistat, since these medications can raise levels of calcium channel blocker drugs; electrocardiographic monitoring is recommended if a calcium channel blocker is used with either atazanavir or saquinavir.[91,92]
Hyperlipidemia
Overview
Combined data from the CDC and NHANES shows that approximately 11.5% of United States adults 20 years of age and older have elevated total cholesterol (defined as greater than or equal to 240 mg/dL), and 27.8% had a low-density lipoprotein cholesterol (LDL-C) level greater than or equal to 130 mg/dL.[69] Elevated cholesterol can lead to atherosclerotic cardiovascular disease, the leading cause of preventable death in the United States.
Lipid-Lowering Agents
Statins remain the primary initial drug class used to treat elevated LDL cholesterol, but multiple different classes of lipid-lowering agents are now available.
- Statins (HMG-CoA Reductase Inhibitors): The statin class of medication works by inhibiting cholesterol synthesis. Specifically, these medications inhibit 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, an enzyme responsible for converting HMG-CoA to mevalonic acid—a key step in cholesterol synthesis.[81] In addition, statins also increase the number of low-density lipoprotein (LDL) receptors.[81] For treatment purposes, statins are categorized based on their impact on lowering LDL cholesterol (LDL-C).[81] Note that some statins have more than one intensity classification based on dose-dependent potency. Statins have the potential to cause hepatotoxicity, myopathy, and new onset of diabetes mellitus.
- Cholesterol Absorption Inhibitors: Ezetimibe is the only approved medication in this class, and it targets the Niemann–Pick C1–like 1 (NPC1L1) protein and thereby selectively inhibits intestinal and biliary cholesterol absorption. The reduced cholesterol absorption causes decreased delivery of intestinal cholesterol to the liver and lowers circulating levels of cholesterol. This medication is also likely to increase the number of LDL receptors. The recommended dose of ezetimibe is 10 mg once daily; it is generally well tolerated, and, in combination with a statin, it lowers LDL cholesterol by an additional 15 to 20% but raises high-density lipoprotein (HDL) cholesterol minimally (about 1 to 2%).[81,93,94] When used, it is typically given in combination with a statin.
- Bile Acid Sequestrants: These agents are large molecular weight polymers that bind to bile acids and bile salts in the intestines, forming an insoluble complex that is excreted in stool. Commonly used bile acid sequestrants include cholestyramine, colesevelam, and colestipol; these medications lower LDL-C by about 15 to 30%.[81] Since these medications are not systemically absorbed, they are generally considered safe, but they can cause bloating and gastrointestinal discomfort. These medications should not be used in someone with biliary obstruction, severe constipation, or severe hypertriglyceridemia.
- PCSK9 Inhibitors: The PCSK9 inhibitors are injectable humanized monoclonal antibodies that bind to proprotein convertase subtilisin–kexin type 9 (PCSK9) and thereby decrease the degradation of LDL receptors.[95,96] At the surface of hepatocytes, the LDL receptors act as binding sites for circulating LDL cholesterol—a key step for processing and removal of LDL. Within the hepatocytes, the LDL receptors have a recycling process whereby they either return to the cell surface or they are shunted to the lysosome and degraded.[96] The enzyme PCSK9 enhances the movement of the LDL receptors to the lysosome. Accordingly, the PCSK9 inhibitors reduce the impact of PCSK9 on LDL receptors being shunted to lysosomes, effectively creating more LDL receptors at the surface of the hepatocyte.[97] This class of medications includes alirocumab and evolocumab; both of these agents are very potent, lowering LDL cholesterol by about 40 to 60%.[81,98] Although PCSK9 inhibitors are potent, safe, and dosed infrequently, they require subcutaneous injections and are very expensive.[96,98]
- Fibrates (PPAR Agonists): The fibrates—derivatives of fibric acid—exert their action as an agonist of peroxisome proliferator-activated receptor alpha (PPAR-α), a protein that increases gene transcription of proteins that regulate metabolism of triglycerides and HDL.[99,100] Fibrates can lower triglycerides by approximately 40% and increase HDL by 15%, but they have minimal impact on LDL levels. Commonly used fibrates include bezafibrate, clofibrate, fenofibrate, and gemfibrozil.
Guidelines for the Management of Dyslipidemia
The 2018 ACC/AHA Cholesterol Treatment Guidelines are the most important guidelines for the management of hyperlipidemia.[81] These guidelines discuss multiple factors to consider when deciding whether to initiate lipid-lowering treatment, including prior ASCVD event, age, LDL-C levels, high-risk conditions, and estimated 10-year risk for heart disease (using the American College of Cardiology ASCVD Risk Estimator).[81]
Baseline Evaluation and Initiation of Therapy
Evaluation for secondary causes of hyperlipidemia should be considered, particularly in persons with severe elevations of LDL (greater than or equal to 190 mg/dL) or triglycerides (greater than or equal to 500 mg/dL). Major secondary causes that are encountered in clinical practice include diet, medications (diuretics, cyclosporine, glucocorticoids, and amiodarone), medical diseases (biliary obstruction or nephrotic syndrome), and disorders of altered metabolism (hypothyroidism, obesity, pregnancy, and diabetes). For patients meeting the criteria for benefit from statin therapy, the guidelines specify whether a high-, moderate-, or low-intensity statin should be initiated, depending on age, calculated ASCVD risk, LDL-C level, and other clinical factors (Figure 7).[101]
Secondary Prevention in Persons with Clinical ASCVD
All persons with clinical ASCVD should receive counseling for optimizing a healthy lifestyle, and all should receive secondary prevention with lipid-lowering therapy.[81] In general, the initial goal of statin therapy for secondary prevention in persons with ASCVD is to achieve a 50% or greater reduction in LDL-C levels and an absolute LDL-C level of less than 70 mg/dL.[81] The following summarizes key recommendations in the guidelines for secondary prevention in persons with ASCVD; detailed recommendations are given in the guidelines.[81] Persons considered to be at very high risk include those with a history of multiple major ASCVD events or 1 major ASCVD event and multiple high-risk conditions.
- Age 75 Years and Younger (and Not at Very High Risk): Initiate therapy with a high-intensity statin; if the high-intensity statin is not tolerated, then use a moderate-intensity statin. If, while on statin therapy, the LDL-C remains at 70 mg/dL or greater, consider adding ezetimibe.
- Age Older than 75 Years (and Not at Very High Risk): Initiate therapy with a moderate- or high-intensity statin.
- Very High Risk (Regardless of Age): Individuals who meet the criteria for very high risk of having a future ASCVD event should initially receive a high-intensity or maximally-tolerated statin. If, while on statin therapy, the LDL-C remains at 70 mg/dL or greater, adding ezetimibe is reasonable. If the LDL-C remains at 70 mg/dL or greater while on a high-intensity statin and ezetimibe, it is reasonable to consult with a lipid specialist when considering adding a PCSK9 inhibitor.
Primary Prevention in Adults
The following summarizes key recommendations from the 2018 ACC/AHA Cholesterol Treatment Guidelines regarding lipid management for primary prevention of ASCVD.[81] In general, the target LDL-C goals for primary prevention are not as stringent as with secondary prevention.[81] Detailed explanations and recommendations are contained in the guidelines.[81] The following highlights key recommendations in these guidelines.
- LDL-C of 190 mg/dL or Greater: For individuals with an LDL-C of 190 mg/dL or greater, therapy can be initiated with a high-intensity statin. Further management of these individuals is based on age and response to therapy.
- Diabetes Mellitus: For persons with diabetes mellitus aged 40 to 75 years, initiate therapy with a moderate-intensity statin, but consider using a high-intensity statin if the individual has multiple ASCVD risk factors. Consider adding ezetimibe if the 10-year ASCVD risk is greater than 20%. For persons with diabetes who are older than 75 years of age, it is reasonable to continue statin therapy, but the decision to initiate statin therapy at this age should be based on a discussion between the medical provider and the patient.
- LDL-C of 71 to 189 mg/dL and Age 40 to 75 Years, without Diabetes: For this group of individuals, the most important first step is to estimate the 10-year ASCVD risk using the American College of Cardiology ASCVD Risk Estimator. In addition, it is important to evaluate for any ASCVD risk enhancers that exist. These recommendations are based primarily on the following 10-year risk categories: low risk (less than 5%), borderline risk (5% up to 7.5%), intermediate risk (7.5% up to 20%), and high risk (20% or greater). In general, the higher the 10-year ASCVD risk category and the greater number of concomitant ASCVD risk enhancers, the more likely that treatment with a statin should be recommended.Table 5. 2018 American College of Cardiology/American Heart Association Guideline on the Management of Blood Cholesterol
Atherosclerotic Cardiovascular Disease (ASCVD) Risk Enhancers
Clinical Factors • Family history of premature ASCVD • Persistent elevated LDL-C ≥160 mg/dL (≥4.1 mmol/L) • Chronic kidney disease • Metabolic syndrome • Conditions specific to women (e.g. preeclampsia, premature menopause) • Inflammatory Diseases (especially rheumatoid arthritis, psoriasis, HIV) • Ethnicity (e.g. South Asian ancestry) Lipid/Biomarkers • Persistently elevated triglycerides (≥175 mg/dL, [≥2.0 mmol/L]) Heterozygous familial hypercholesterolemia • Elevated high-sensitivity C-reactive Protein (CRP) ≥2.0 mg/L • Lipoprotein (a) levels ≥50 mg/dL (or ≥125 nmol/L) • apoB ≥130 mg/dL • Current smoking • Ankle-brachial index (ABI) <0.9 Abbreviations: ASCVD = atherosclerotic cardiovascular disease; LDL-C = low density lipoprotein cholesterol; hs-CRP = high sensitivity C-reactive protein Source:- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143. [PubMed Abstract]
Management of Hypertriglyceridemia
Elevated triglycerides can also increase the risk of cardiovascular disease. The 2018 ACC/AHA Cholesterol Treatment Guidelines outline two categories of elevated triglycerides: (1) moderate hypertriglyceridemia (fasting or nonfasting triglycerides 150 to 499 mg/dL) or (2) severe hypertriglyceridemia (fasting triglycerides 500 mg/dL or greater).[81] The following summarizes key general recommendations from the 2018 ACC/AHA Cholesterol Treatment Guidelines regarding lipid management for primary prevention of ASCVD.[81]
- Adults 20 Years of Age and Older and Fasting or Nonfasting Triglyceride Level 175 to 499 mg/dL: Clinicians should address and modify lifestyle factors as needed and optimally manage secondary factors, such as diabetes mellitus, chronic liver or kidney disease, or hypothyroidism. In addition, any medication that may increase triglycerides should, if possible, be stopped.
- Adults 40 to 75 years of age with Moderate or Severe Hypertriglyceridemia and ASCVD risk of 7.5% or Higher: The guidelines suggest it is reasonable to reevaluate the ASCVD after the individual addresses lifestyle and secondary factors; if triglycerides are persistently elevated, consider initiation or intensification of statin therapy.
- Adults 40 to 75 years of age with Severe Hypertriglyceridemia and ASCVD risk of 7.5% or Higher: A reasonable approach is to address any potential reversible causes of hypertriglyceridemia and initiate lipid-lowering therapy with a statin.
- Adults with Severe Hypertriglyceridemia, especially Fasting Triglyceride Levels of 1,000 mg/dL or Greater: The guidelines suggest it is reasonable to first address other causes of hypertriglyceridemia; if triglyceride levels remain elevated or increase, then implement a very low-fat diet, avoid alcohol and refined carbohydrates, increase consumption of omega-3 fatty acids, and start fibrate therapy if necessary to prevent pancreatitis.
Special Considerations for People with HIV
Persons with HIV are estimated to have a 1.5 to 2-fold greater risk of developing ASCVD and at an earlier incident age.[102] The AIDS Clinical Trials Group (ACTG) Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE) trial was a randomized, double-blind, international trial that enrolled 7,769 participants with HIV and low-to-moderate risk of cardiovascular disease to receive pitavastatin 4 mg or placebo.[103] The major goal of the study was to test whether statin therapy reduces the risk for major adverse cardiovascular events in persons with HIV.[103] The trial was stopped early because persons in the pitavastatin group had 35% fewer adverse cardiovascular events compared with those receiving a placebo after a median follow-up of 5.1 years.[103] The Adult and Adolescent ART Guidelines issued new guidance on the use of statins in persons with HIV as primary ASCVD prevention in February 2024, based on findings of the AIDS Clinical Trials Group (ACTG) Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE) Trial.[102,103] In general, the approach to secondary prevention of ASCVD in persons with HIV is the same as in persons without HIV.
Mechanism of Lipid Disorders Associated with HIV
The pathophysiology of cardiovascular disease and dyslipidemia in HIV is multifactorial—it has been associated with traditional risk factors, such as hypertension, diabetes mellitus, dyslipidemia, family history, and tobacco use, as well as with HIV itself and antiretroviral therapy.[50,56] Effective antiretroviral therapy does not completely nullify the adverse cardiovascular impact from HIV, but it does significantly reduce it. Chronic HIV can lead to abnormalities in lipid levels, vascular stiffness, inflammation, and immune activation, even with effective antiretroviral therapy and virologic suppression.[104] Compared to individuals without HIV, people with HIV have been shown to have a higher prevalence of atypical, high-risk, noncalcified coronary plaques.[50,104]
Effect of Antiretroviral Therapy on Lipids
Different antiretroviral therapies have distinct effects on lipid levels, with protease inhibitors generally causing the greatest increases (especially LDL and triglycerides) and integrase strand transfer inhibitors (INSTIs) exerting the least lipid effect; within classes, certain agents are recognized to cause more adverse lipid effects than others (Figure 8).[105,106] If an individual with HIV has abnormal lipid levels while taking antiretroviral therapy, a review of the antiretroviral regimen should be performed to identify medications that may be contributing to lipid abnormalities, particularly efavirenz, protease inhibitors, and boosting agents (ritonavir and cobicistat).[53] Modern preferred unboosted INSTI-based antiretroviral regimens generally do not adversely impact lipid parameters, and switching to an INSTI-based regimen from a boosted-protease inhibitor can improve lipids.[107,108] Tenofovir DF, but not tenofovir alafenamide, typically lowers LDL and triglyceride levels.[109] If a decision is made to change a patient’s existing antiretroviral therapy regimen to a more “lipid-friendly” antiretroviral regimen, the goal of maintaining viral suppression is paramount, and current and archived resistance mutations must be taken into consideration when deciding on the new regimen.[106,110]
Routine Monitoring of Lipid Profiles in People with HIV
The following summarizes recommendations for monitoring lipid profiles in people with HIV.[111]
- Entry into Care: At the time of entry into HIV care, a lipid profile should be ordered; if the test performed was a random lipid profile and it is abnormal, then a fasting lipid panel should be ordered.
- Antiretroviral Initiation or Modification: A lipid profile should be ordered at the time of initiating or changing antiretroviral therapy.
- After Initiation or Modification of Antiretroviral Therapy: Consider ordering a lipid profile 4 to 8 weeks after initiating or modifying antiretroviral therapy.
- Routine Monitoring: If the lipid profile is abnormal or the person has cardiovascular risk, then monitoring should be conducted every 12 months. If the lipid profile remains normal and there is no cardiovascular risk, then monitoring should be every 5 years.
- Persons on Lipid-Lowering Therapy: Persons receiving lipid-lowering therapy should have lipid monitoring individualized, and more frequent monitoring may be needed.
Primary Prevention of ASCVD in People with HIV
The following summarizes recommendations in the Adult and Adolescent ART Guidelines for the use of statins in persons with HIV as primary prevention of ASCVD.[102]
Age 40-75 Years and Low-to-Intermediate (<20%) 10-Year ASCVD Risk Estimates:
- If ASCVD 5-20%, start at least moderate-intensity statin (AI)
- Pitavastatin 4 mg orally once daily (AI), or
- Atorvastatin 20 mg orally once daily (AII), or
- Rosuvastatin 10 mg orally once daily (AIII)
- If ASCVD <5%, the guidelines favor starting at least moderate-intensity statin therapy, after shared decision-making taking into account the presence or absence of HIV-related factors that can increase ASCVD risk (CI)
- Pitavastatin 4 mg orally once daily (AI), or
- Atorvastatin 20 mg orally once daily (AII), or
- Rosuvastatin 10 mg orally once daily (AIII)
Age Younger than 40 years
- Data are insufficient to recommend for or against statin therapy as primary prevention of ASCVD in persons younger than 40 years of age.
Lifestyle Optimization and Management of Other Risk Factors
All people with HIV should receive counseling on lifestyle optimization that includes smoking cessation, eating a cardiac-healthy diet, engaging in regular exercise, and limiting alcohol intake to less than 7 drinks per week.[53] In addition, management of other factors that influence ASCVD, including hypertension and diabetes mellitus, should be optimized.[53]
Drug Interactions with Antiretroviral Medications and Lipid-Lowering Therapies
Careful review of the patient’s antiretroviral therapy regimen for possible drug interactions should guide the decision of which statin to start in persons with HIV. In general, low-dose atorvastatin, pitavastatin, and rosuvastatin are unlikely to have significant drug interactions with antiretroviral medications.[112] Potentially dangerous drug interactions can occur between some statins and HIV antiretroviral medications, particularly with HIV PIs, NNRTIs, and the pharmacologic boosters ritonavir and cobicistat.[16,84,91,106,113,114] For example, ritonavir and cobicistat can dramatically increase serum levels of simvastatin and lovastatin, thus increasing the risk of statin-related hepatotoxicity, myopathy, and rhabdomyolysis. For this reason, simvastatin and lovastatin are contraindicated in combination with ritonavir- or cobicistat-containing regimens. Conversely, the NNRTI efavirenz induces statin metabolism and may decrease the efficacy of some statins.[114]
Monitoring for Treatment Response and Adverse Effects
The 2019 AHA Statement on CVD and HIV does not give a target goal for treatment response whereas the 2018 ACC/AHA Cholesterol Treatment Guidelines recommend using a goal of 50% or greater reduction in LDL-C levels. Once the statin is started, a lipid panel should be checked 4 to 12 weeks after initiation to assess for treatment response, with the goal to slowly titrate up the statin dose if needed to achieve the target LDL level. Following this, lipids should be checked every 6 months if abnormal and once yearly if stable. The statins have the potential to cause muscle and liver toxicity, especially when used at high doses. The dose of the statin should be decreased, or the medication discontinued if the person taking a statin experiences any of the following: severe muscle aches (or unexplained muscle weakness), an increase in serum creatine kinase to greater than 10 times the upper limit of normal, or an increase in hepatic aminotransferase levels that exceeds 3 times the upper limit of normal.[53] Statin therapy is not recommended if a person is pregnant or breastfeeding.[102]
Use of Nonstatin Therapies in People with HIV
The use of nonstatin therapies may be considered in persons with HIV in the following situations: (1) as adjunctive therapy in combination with a statin in persons who have high cardiovascular risk, (2) in persons who are intolerant of statins, and (3) in persons who fail to respond adequately to statins. In patients with familial hyperlipidemia, a high-dose statin, then ezetimibe, and last, a PCSK9 inhibitor can be tried with expert consultation and guidance if LDL levels remain elevated despite maximal therapy. The use of ezetimibe or PCSK9 inhibitors is limited mainly to secondary prevention in persons at very high risk of an ASCVD event or those who have not experienced an adequate response to statin therapy.[81].
- Cholesterol Absorption Inhibitor: The use of oral ezetimibe, a cholesterol absorption inhibitor, has been studied in people with HIV and can be considered.[115,116,117] Although no specific guidelines exist for the use of ezetimibe in persons with HIV, it is reasonable to utilize a similar approach as for people without HIV, mainly using this medication as an adjunct to statin therapy in people who do not adequately respond to or cannot tolerate statin therapy.[81]
- Proprotein Convertase Subtilisin/Kexin type 9 (PCSK9) Inhibitors: There are sparse data on the safety and efficacy of PCSK9 inhibitors in persons with HIV. An ongoing trial—the Effect of PCSK9 Inhibition on Cardiovascular Risk in Treated HIV Infection (EPIC-HIV)—is evaluating the impact of PCSK9 inhibitors on lipid levels, subclinical ASCVD, and inflammatory markers in persons with HIV.
Treatment of Hypertriglyceridemia in People with HIV
Elevated triglyceride levels are common among people with HIV. Several studies in large cohorts of people with HIV have demonstrated that triglyceride levels did not predict cardiovascular disease or were associated with marginally elevated ASCVD risk.[53,118,119] Although hypertriglyceridemia likely does not play a major role in ASCVD risk in people with HIV, treatment of severe hypertriglyceridemia (fasting triglyceride levels above 500 mg/dL) is important to prevent acute pancreatitis. An evaluation should take place for secondary causes of hypertriglyceridemia, such as diabetes mellitus, chronic liver disease, kidney disease, nephrotic syndrome, hypothyroidism, and medications with a known impact of increasing triglyceride levels. If the antiretroviral regimen includes one or more medications that are likely to elevate triglyceride levels, consideration should be given to changing the regimen. Since there are no guidelines for the management of hypertriglyceridemia in persons with HIV, we recommend following the general recommendations in the 2018 ACC/AHA Cholesterol Treatment Guidelines, as summarized above.[81]
Osteoporosis
Overview
An estimated 53 million men and women in the United States have osteoporosis or low bone density, and up to 50% of postmenopausal White women and 20% of men suffer an osteoporosis-related fracture during their lifetime.[120,121,122,123] The USPSTF reported that by 2020 an estimated 12.3 million people in the United States who are older than 50 years of age will have osteoporosis.[120] Osteoporosis is associated with chronic pain, disability, decreased quality of life, and increased mortality.
Risk Factors for Osteoporotic Fractures
Key risk factors for osteoporotic fractures include increasing age, low body weight, female sex, postmenopause for women, parental history of osteoporotic fracture, current tobacco use, excessive alcohol consumption, rheumatoid arthritis, vitamin D deficiency, low calcium intake, history of falls, and immobilization.[120,122] In addition, osteoporosis risk increases with prolonged exposure to certain medications, such as glucocorticoids, anticoagulants, anticonvulsants, aromatase inhibitors, cancer chemotherapeutic drugs, and gonadotropin-releasing hormone agonists.[121] Further, rates of osteoporotic fractures are higher in White than Black individuals.[122,123]Screening for Osteoporosis
There is convincing evidence that screening for osteoporosis has predictive value for osteoporotic fractures in both women and men, and therapies are available to reduce fracture risk. Most commonly, screening is performed with the measurement of bone mineral density by dual-energy x-ray absorptiometry (DXA) of the hip and lumbar spine. In addition, the University of Sheffield, UK, developed the Fracture Risk Assessment (FRAX) tool, often referred to as the FRAX Calculation Tool, to estimate 10-year osteoporotic fracture risk based on age, race, body mass index (BMI), secondary causes of osteoporosis, personal and parental fracture history, tobacco and alcohol use, and previous DXA results if available. If previous DXA results are not available, the calculator can still be used. The FRAX tool has been studied throughout the world and provides country-specific risk assessment, which can be used to select appropriate candidates for osteoporosis screening and treatment.
Current Guidelines
Screening Recommendations
In the general population, the 2018 USPSTF Osteoporosis Screening Guidelines provide recommendations for three groups of adults: (1) women 65 years of age and older, (2) postmenopausal women younger than 65 years of age, and (3) men.[120]
- Women 65 Years of Age and Older: Screening for osteoporosis should be performed in all women 65 years of age and older. A DXA scan is most commonly used for screening.
- Postmenopausal Women Younger than 65 Years of Age: Screening for osteoporosis is recommended for postmenopausal women younger than 65 years of age who are at increased risk of osteoporosis, as determined by a clinical risk assessment tool, such as the FRAX Calculation Tool. More specifically, these guidelines recommend using the risk assessment tool for postmenopausal women younger than 65 who have at least one of the following risk factors for developing osteoporosis: parental history of hip fracture, smoking, excessive alcohol consumption, or low body weight.
- Men: There is no recommendation for or against screening for osteoporosis in men due to insufficient data. Note that guidelines issued by the National Osteoporosis Foundation recommend that all men 70 years of age and older and men 50 to 69 years of age with increased risk for osteoporosis should undergo bone mineral density screening with a DXA scan.[121]
Management Recommendations
In 2017, the American College of Physicians (ACP) released an evidence-based clinical practice guideline titled Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women.[122]
- Treatment of Osteoporosis in Women: The ACP guidelines recommend treatment of women with osteoporosis using bisphosphonates (including alendronate, risedronate, or zoledronic acid) or denosumab therapy and avoiding hormonal therapy or selective estrogen receptor modulators.[122] Treatment should generally be discontinued after 5 years. Monitoring for the progression of osteoporosis during treatment is not recommended. Continuing treatment after the initial 5 years is controversial, but may be beneficial for some women, particularly those whose bone mineral density remains in the osteoporotic range after 5 years of treatment.[124,125]
- Treatment of Osteoporosis in Men: Treatment of men with osteoporosis should primarily involve bisphosphonates, though data is limited in this population.[122]
- Treatment of Osteopenia in Women and Men: The ACP guideline also addresses the complexities of treating women with osteopenia, and it recommends engaging women 65 years of age or older who are at high risk for fracture (e.g., T-score between -2.0 and -2.5) in a discussion of risks and benefits of treatment, taking into account individual patient preferences and fracture risk profile.[122] The National Osteoporosis Foundation more specifically recommends initiating treatment in women and men with osteopenia 50 years of age and older with a 10-year hip fracture risk greater than or equal to 3% or a 10-year major osteoporosis-related fracture risk greater than or equal to 20% based on the United States FRAX tool.[121]
Special Considerations for Persons with HIV
Lower bone density is more prevalent among persons with HIV, and this may be related to factors that are unique to persons with HIV, including increased inflammation, altered bone metabolism, and toxicities related to antiretroviral medications.[126,127] Initiation of antiretroviral therapy has been associated with a 2 to 6% decrease in bone mineral density during the first 2 years of therapy, which varies with the specific antiretroviral regimen used: tenofovir DF and boosted protease inhibitors, in particular, have been linked to greater loss of bone density compared with other antiretroviral agents.[128,129] In contrast, tenofovir alafenamide does not cause significant loss of bone mineral density.[130,131] The following summarizes recommendations from the HIVMA/IDSA Primary Care Guidance and the Recommendations for Evaluation and Management of Bone Disease in HIV.[16,128]
Screening Recommendations for Persons with HIV
- All postmenopausal women with HIV and men 50 years of age and older with HIV should undergo bone mineral density screening with a DXA scan.[16] Bone mineral density should also be assessed with a DXA scan in all adults with HIV who have a major risk factor for fragility fracture, including personal history of fragility fracture, chronic glucocorticoid treatment (greater than or equal to 5 mg of prednisone daily or equivalent for at least 3 months), or high risk of falls.
- In men with HIV 40 to 49 years of age and premenopausal women with HIV 40 years of age and older without a major risk factor for osteoporotic fracture, clinicians should assess fracture risk using the Fracture Risk Assessment Tool (FRAX Calculation Tool) specific to their country and the patient’s race/ethnicity. Risk assessment should be performed every 2 to 3 years or when a new clinical risk factor develops.
- When using the FRAX tool, some experts recommend checking the “secondary osteoporosis” box to better adjust the estimate, considering the increased risk of osteoporosis conferred by HIV. A DXA scan should be performed if the FRAX tool determines the 10-year risk of major osteoporotic fracture to be greater than 10%.
- When interpreting DXA results, use T-scores for postmenopausal women and men 50 years of age and older and use Z-scores for persons younger than 50 years of age.
- Optimal screening intervals (for DXA or FRAX assessment) are not clear for persons with HIV. Consider repeating a DXA scan after 1 to 2 years for individuals who have advanced osteopenia (T-score -2.0 to -2.49) and after 5 years in those with mild-to-moderate osteopenia (T-score of -1.01 to -1.99); for those who have a normal DXA, guidance on when to repeat screening is not given.
- Vitamin D screening is recommended in all individuals with low bone mineral density or history of a fragility fracture; it should be considered in persons who have any of the major known risk factors for low vitamin D levels (e.g., dark skin, dietary deficiency, avoidance of sun exposure, malabsorption, obesity, chronic kidney disease, or treatment with regimens containing efavirenz).
- Routine measurement of serum or urine markers of bone turnover or inflammation for screening or treatment monitoring is not recommended for persons with HIV.
Management Recommendations for Persons with HIV
- Persons with osteoporosis (or at risk of osteoporosis) should, if possible, avoid tenofovir DF and boosted protease inhibitors.
- For individuals at high risk for osteoporosis, dietary management strategies should be employed, which include ensuring adequate calcium intake and, if indicated, vitamin D supplementation.
- Vitamin D supplementation should be titrated to a target serum 25-hydroxy vitamin D level of approximately 30 ng/mL or higher.
- Lifestyle modifications for persons with osteopenia or osteoporosis include regular weight-bearing and muscle-strengthening exercises, avoidance of falls, smoking cessation, and reduction in alcohol consumption.
Additional Evaluation for Persons with HIV
- For persons with HIV who have osteopenia or osteoporosis, possible treatable secondary causes for decreased bone mineral density should be identified and addressed; these secondary causes include smoking, alcohol use, sedentary lifestyle, low BMI, exposure to medications associated with bone loss (glucocorticoids, phenytoin, proton pump inhibitors, thiazolidinediones), vitamin D deficiency, renal disease, hyperparathyroidism, thyroid disease, and hypogonadism. If the person has osteopenia and a reversible secondary cause, the underlying cause should be addressed without a bisphosphonate, if possible, and a repeat DXA should be obtained within 1 year.[16]
- It is important to rule out osteomalacia (softening of the bones due to demineralization, which can be caused by tenofovir DF-induced renal phosphate wasting and/or vitamin D deficiency) before treating with bisphosphonates; low vitamin D and calcium supplementation can also blunt the response to bisphosphonates and ideally should precede initiation of bisphosphonate therapy.
Pharmacotherapy Recommendations
- In general, the management of osteopenia or osteoporosis in persons with HIV should follow established guidelines for the general population without HIV; several exceptions exist, as outlined below.[128]
- In 2017, the American College of Physicians (ACP) released an evidence-based clinical practice guideline titled Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women, which recommends initiating pharmacotherapy in women and men with osteoporosis.[122] The guideline also addresses the complexities of treating women with osteopenia, and it recommends engaging women 65 years of age or older who are at high risk for fracture (i.e., T-score between -2.0 and -2.5) in a discussion of the risks and benefits of treatment. The National Osteoporosis Foundation more specifically recommends initiating treatment in women and men with osteopenia 50 years of age and older who have an estimated 10-year hip fracture risk greater than or equal to 3% or a 10-year major osteoporosis-related fracture risk greater than or equal to 20% (based on the FRAX Calculation Tool for persons in the United States).[121]
- When therapy is indicated for persons with HIV at risk for osteoporotic fractures, the use of alendronate or zoledronic acid is preferred, since other therapies have not been adequately studied in persons with HIV. This differs from the 2017 ACP guideline, which also includes risedronate and denosumab as possible initial drugs of choice in the general population.[122]
- Treatment duration should be individualized, though the 2017 ACP guideline recommends discontinuing treatment after 5 years in the general population.[122]
- Bisphosphonates have been associated with adverse effects, including esophagitis, osteonecrosis of the jaw, and atypical femoral fractures; patients on these medications should be monitored clinically for these outcomes.[132,133]
- Some experts would repeat a DXA scan after 3 to 5 years of pharmacotherapy. For individuals with worsening bone mineral density, a new fracture, greater than 1 cm of height loss, or poor adherence to oral bisphosphonate therapy, alternate treatment, including intravenous zoledronic acid or teriparatide could be considered, though data are limited with teriparatide and other osteoporosis pharmacotherapies in persons with HIV.
- Individuals receiving bisphosphonates with evidence of worsening bone mineral density, new fractures, suspected osteomalacia, or intolerance of treatment may benefit from referral to a bone health specialist.
Drug Interactions
Drug interactions are not expected with concurrent bisphosphonate and antiretroviral therapy, but caution should be used if calcium supplementation is administered in the form of an antacid such as calcium carbonate, as polyvalent cations can interfere with the absorption of atazanavir, bictegravir, dolutegravir, elvitegravir, and rilpivirine.[84,91,114] Calcium-containing antacids must be separated from some antiretroviral medications, and prescribing information for the specific antiretroviral medication should be followed.[84]
Renal Disease
Overview
Based on NHANES data collected from 2015 through 2018, the overall prevalence of chronic kidney disease (CKD) among adults in the United States older than 20 years was approximately 15%.[69] The 2012 KDIGO Clinical Practice Guideline defines chronic kidney disease as abnormalities of kidney structure or function present for greater than 3 months, with implications for health.[134] Historically, in 2002, the National Kidney Foundation–Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) proposed a chronic kidney disease staging system based on glomerular filtration rate (GFR) stages 1 through 5 (Figure 9).[135,136] The 2012 KDIGO Clinical Practice Guideline recommends classifying chronic kidney disease by cause, glomerular filtration rate category, and albuminuria category in recognition that GFR and albuminuria are complementary and independent predictors of important clinical outcomes, including CKD progression, end-stage renal disease, and all-cause mortality (Figure 10).[134]
Special Considerations for Persons with HIV
In persons with HIV, the risk of developing chronic kidney disease is higher in individuals who are older in age, female, or Black and in those who have CD4 counts less than 200 cells/mm3, elevated HIV RNA levels, or comorbid conditions such as diabetes, hypertension, and hepatitis C.[83] Earlier in the HIV epidemic in the United States, HIV-related kidney disease predominantly resulted from sequela of HIV infection, such as with HIV-associated nephropathy (HIVAN) or immune complex disease; these disorders most often occurred in persons with untreated HIV, particularly those with a low CD4 cell count.[137,138] In the current era, since most people with HIV achieve virologic suppression on antiretroviral therapy and have a near normal expected lifespan, the cause of renal disease has shifted from HIV-related disease to chronic comorbid conditions, such as hypertension, diabetes, or chronic hepatitis C virus (HCV) infection.[137,138] In addition, certain antiretroviral agents, such as tenofovir DF, can play a role in causing chronic kidney disease in persons with HIV. If chronic kidney disease develops, it has significant implications for cardiovascular disease and all-cause mortality.
Guidelines and Recommendations for Persons with HIV
The HIV Medical Association (HIVMA) has provided a comprehensive HIVMA CKD Clinical Practice Guideline that addresses renal disease among persons with HIV, and it provides management recommendations.[83] Staging for chronic kidney disease in the HIVMA CKD Clinical Practice Guideline follows the KDIGO definitions outlined above.[83] The following summarizes key recommendations regarding the evaluation, management, and prevention of renal disease in persons with HIV, with an emphasis on recommendations in the Adult and Adolescent ART Guidelines and the HIVMA CKD Clinical Practice Guideline.[83,111]
Baseline Evaluation and Routine Monitoring for Renal Disease
- Persons with HIV should have a creatinine-based estimated glomerular filtration rate (eGFR) at the time of HIV diagnosis, when antiretroviral therapy is initiated or changed, and twice a year as long as renal function remains normal.[83,111]
- Persons with HIV should have a urinalysis at entry into care.[111] In addition, urine glucose and urine protein should be assessed prior to starting an antiretroviral regimen that contains tenofovir DF or tenofovir alafenamide, and it should be monitored while receiving either of these medications.[111] Proteinuria of 1+ or greater on urinalysis should be quantified with either an albumin-to-creatinine ratio (often called a urine microalbumin test) or a protein-to-creatinine ratio. Both the albumin-to-creatinine ratio and protein-to-creatinine ratio can be obtained from a spot urine sample or from a 24-hour urine collection.
- The HIVMA/IDSA Primary Care Guidance provides a more liberal recommendation by suggesting that the frequency of monitoring for renal function, such as with chemistry panels and urinary abnormalities, depends on the need to monitor for antiretroviral toxicities and the presence of underlying medical conditions that can increase risk of CKD, including diabetes, hypertension, HCV, nephrotoxic medications, genetic predisposition, or advanced HIV disease.[16] In those taking tenofovir DF, biannual monitoring for renal function and urinary abnormalities is recommended. Otherwise, urinalysis should be monitored annually among those at risk for kidney disease.[16]
- Workup for new-onset kidney disease in persons with HIV should include serum chemistry panel, urinalysis, quantitative measure of albuminuria, assessment of glucose and blood pressure control, markers of proximal tubular dysfunction, renal sonogram, and medication review to determine any agents that may be nephrotoxic or require renal dosing.
Referral for Persons with HIV and Renal Impairment
- Persons with HIV should be referred to a nephrologist if GFR declines more than 25% from baseline and to a level less than 60 mL/min/1.73 m2 that fails to resolve with the removal of any potential nephrotoxic drugs.[83] Additional indications for referral include albuminuria greater than 300 mg/day, hematuria with either proteinuria or elevated blood pressure, and advanced kidney disease with GFR less than 30 mL/min/1.73 m2.
- Individuals with HIV and end-stage renal disease should undergo evaluation for their potential candidacy for renal transplantation.
HIV-Associated Nephropathy (HIVAN)
All individuals with HIV-associated nephropathy (HIVAN) should receive treatment with effective antiretroviral therapy at diagnosis.[83,137] Antiretroviral therapy should not be withheld due to the severity of renal dysfunction or low CD4 cell count. For refractory HIVAN, treatment may include an ACE inhibitor or ARB, and possibly also corticosteroids.[83,137]
Antiretroviral Therapy and Chronic Kidney Disease
Certain antiretroviral agents can cause nephrotoxicity, usually through tubular injury with tenofovir DF or crystal nephropathy from atazanavir or indinavir.[138,139,140,141]. Antiretroviral therapy-related nephrotoxicity from tenofovir DF most frequently involves proximal tubular nephropathy, which can progress to Fanconi syndrome.[137] Several studies suggest that the risk for tenofovir DF-related kidney injury increases in the setting of older age, lower body weight, diabetes, hypertension, and with concomitant use of a PI, particularly ritonavir-boosted protease inhibitors.[83,142] With antiretroviral-associated nephrotoxicity, full renal recovery does not always occur after withdrawal of the offending drug. Tenofovir DF (and any coformulations that include tenofovir DF) should, if feasible, be avoided in persons with a baseline GFR less than 60 mL/min/1.73 m2.[83] If tenofovir DF is used in a person with a creatinine clearance less than 50 mL/min, a dose reduction is required. Tenofovir alafenamide, a prodrug of tenofovir, achieves higher intracellular but lower plasma levels of tenofovir than tenofovir DF. In addition, tenofovir alafenamide is not transmitted into the proximal tubular cells via the organic anion transporters 1 and 3.[137,141] For these reasons, tenofovir alafenamide causes significantly less nephrotoxicity than tenofovir DF.[143] Although tenofovir alafenamide is less nephrotoxic than tenofovir DF, rare cases of nephrotoxicity associated with tenofovir alafenamide have been reported.[144,145,146] Tenofovir alafenamide-emtricitabine is not recommended for persons with a creatinine clearance less than 30 mL/min; tenofovir alafenamide (alone) is not recommended for persons with a creatinine clearance less than 15 mL/min.
Evaluating Tenofovir DF-Associated Nephrotoxicity
For individuals who develop renal dysfunction in the setting of tenofovir DF use, it can be challenging to determine whether tenofovir DF is the cause. Measuring serum or urinary markers of proximal tubular dysfunction may be helpful in this scenario (Figure 11).[83]
- Two indicators are highly specific markers of proximal tubular dysfunction: (1) glycosuria with normal serum glucose and (2) urinary phosphorus wasting with low serum phosphorus. Additional markers that suggest proximal tubular dysfunction include serum parameters (hypokalemia and decreased serum bicarbonate) and urinary abnormalities (urine albumin-to-protein ratio less than 0.4).
- Phosphorus wasting can be determined by fractional excretion of phosphate. Normal fractional excretion of phosphate is generally defined as less than 10%, and impaired fractional excretion of phosphate is defined as above 20%; thus, a fractional excretion of phosphate above 20% raises the likelihood of tenofovir toxicity, whereas a result below 10% makes tenofovir toxicity unlikely.[83] See the Fractional Excretion of Phosphate Calculator in the Tools and Calculators section.
- Proteinuria is not specific for proximal tubular dysfunction but should also be included in the workup because data suggest that a lower albumin-to-protein ratio of less than 0.4 may be useful in distinguishing proteinuria due to proximal tubular dysfunction (secondary to tenofovir toxicity) from proteinuria due to glomerular disease.[83]
Criteria for Discontinuing Tenofovir DF
Regardless of the cause, the HIVMA CKD Clinical Practice Guideline states that tenofovir DF should be discontinued in persons with HIV who experience a decline in GFR greater than 25% and to a level less than 60 mL/min/1.73m2, but this is particularly important when there is evidence that tenofovir DF is the cause (e.g., evidence of proximal tubular dysfunction or new-onset or worsening proteinuria).[83]
Renal Dosing of Antiretroviral Medications
The CKD-Epidemiology collaboration (CKD-EPI) or Cockcroft-Gault equation should be used to estimate creatinine clearance when dosing antiretroviral therapy or other drugs that may require renal dosing. See the Creatinine Clearance Calculator and the Glomerular Filtration Rate (GFR) Calculator in the Tools and Calculator section of this website.
Medications Used in HIV Care that May Cause Benign Elevations in Serum Creatinine
In contrast to tenofovir DF-induced changes in renal function that generally signify kidney damage, the medications bictegravir, cobicistat, dolutegravir, rilpivirine, and trimethoprim may decrease tubular creatinine secretion and raise serum creatinine without altering actual renal function.[16,83] In these settings, a 10 to 20% elevation (or 0.1 to 0.2 mg/dL increase) in serum creatinine may be expected.[147]. Elevations in serum creatinine typically occur in the first few weeks of therapy and subsequently plateau.[148] The additive effect of these medications (e.g., when dolutegravir is combined with rilpivirine) is unclear. After initiation of these medications, a repeat serum creatinine should be obtained within one month to establish a new baseline. If the creatinine is elevated beyond the expected elevation on the first check, repeat the serum creatinine to get a better marker for true renal function.[137,149,150,151]ASCVD Prevention in Persons with HIV and Renal Disease
- Aspirin: Some experts consider people with HIV and chronic kidney disease as candidates for low-dose aspirin (75 to 100 mg/day), though the risk of bleeding and benefits of primary cardiovascular disease prevention should be weighed in the decision process.[83] Note the 2019 ACC/AHA Primary CVD Prevention Guidelinerecommendation against the use of aspirin for primary prevention of ASCVD in adults at any age who are at increased risk of bleeding, including those with chronic kidney disease.[44] In addition, the USPSTF recommends against initiating low-dose aspirin as primary prevention in adults 60 years or older. In adults 40 to 59 years with a 10-year ASCVD risk of 10% or greater, which may be seen in persons with HIV and renal disease, the decision to initiate low-dose aspirin for primary prevention of CVD should be individualized.[42]
- Lipid-Lowering Therapy: In accordance with the 2018 ACC/AHA Cholesterol Treatment Guidelines, chronic kidney disease is considered an ASCVD risk enhancer.[81,152] Accordingly, many persons with HIV and kidney disease will receive statin therapy. Although there are no studies of statin therapy in persons with both HIV and chronic kidney disease, the HIVMA CKD Clinical Practice Guideline cites evidence of statin benefit in persons without HIV who have chronic kidney disease.[83] There is also accumulating evidence that statin therapy slows kidney function decline in persons with HIV on antiretroviral therapy.[153] Because studies of patients with end-stage renal disease (ESRD) on hemodialysis have not shown a reduction in cardiovascular events or mortality from statin therapy, statins are not recommended in this group (regardless of HIV status).
Testosterone Deficiency
Overview
In the male adult population in the United States, testosterone deficiency is common, occurring in approximately 10% of males 18 years of age and older.[154] In the United States and the United Kingdom, trends from 2000-2011 showed that initiation of testosterone therapy increased, despite steady rates in testosterone testing frequency and in laboratory-diagnosed testosterone deficiency.[154]
Testosterone Screening Guidance
The 2018 Endocrine Society Testosterone Therapy Guidelines provide recommendations for testosterone deficiency screening, which are summarized as follows.[155]
Indications for Testosterone Screening
A laboratory workup for testosterone deficiency should only be performed if the person under evaluation has signs or symptoms that suggest testosterone deficiency.[155] Symptoms suggestive of testosterone deficiency include a decrease in libido, infrequent spontaneous erections, erectile dysfunction, fatigue, or depression; signs suggestive of testosterone deficiency include gynecomastia, loss of pubic hair, small testes, low bone mineral density, decreased muscle mass, or incomplete or delayed sexual development.[155] The 2018 Endocrine Society Testosterone Therapy Guidelines recommend against routine screening of men in the general population for hypogonadism.[155]
Optimizing Laboratory Screening for Testosterone Deficiency
- The most accurate testosterone measurements are those obtained in the morning, ideally between 8 and 10 A.M., as testosterone levels peak in the morning and tend to wane over the course of the day.
- A fasting blood draw is ideal, as food intake or glucose may suppress testosterone concentrations, leading to falsely decreased testosterone levels.
- In persons with a condition that can alter sex hormone binding globulin, a free testosterone level should be obtained, in addition to a total testosterone level.
- The testosterone assay used should be one that has been certified with an accuracy-based standardization or quality control program.
- A testosterone level should not be checked during an acute illness or in those who are taking certain medications (e.g., opioids or anabolic steroids) that may suppress testosterone concentrations.
Confirming a Low Testosterone Screening Result
If a fasting morning testosterone level is low, this should be repeated and confirmed. A laboratory diagnosis of testosterone deficiency is made when a person has two documented decreased morning fasting serum testosterone levels. Since low testosterone concentrations often occur without clinical symptoms or signs of testosterone deficiency, a low testosterone level alone does not establish a clinical diagnosis of hypogonadism.[155]
Recommendations for Testosterone Therapy
The 2018 Endocrine Society Testosterone Therapy Guidelines provide recommendations for testosterone therapy for individuals with documented testosterone deficiency, which are summarized as follows.[155]
Indications to Start Testosterone Therapy
If an individual under evaluation has had two decreased morning fasting serum testosterone levels and has signs or symptoms consistent with androgen deficiency (as outlined above), then testosterone therapy is indicated if, after a discussion with the individual that addresses benefits and potential adverse effects, such as erythrocytosis and cardiovascular events, the individual agrees.[156] In addition, prior to initiating testosterone therapy, the clinician should determine whether any contraindications exist for testosterone therapy.Baseline Evaluation Prior to Initiating Testosterone Therapy
- A luteinizing hormone (LH) and follicle hormone (FSH) level should be obtained to distinguish between primary (testicular) and secondary (pituitary-hypothalamic) hypogonadism. An elevated LH and FSH suggest primary hypogonadism, whereas a low or inappropriately normal LH and FSH suggest secondary hypogonadism.
- A hematocrit should be obtained.
- In hypogonadal men 40 years of age and older at high risk for prostate cancer, a prostate-specific antigen (PSA) and digital rectal examination should be offered.
- The patient’s past medical history or problem list should be reviewed to rule out any contraindicating conditions.
Contraindications for Testosterone Therapy
Testosterone therapy should not be given to persons who have any of the following listed disorders:
- Breast or prostate cancer
- A palpable prostate nodule or induration
- Prostate PSA greater than 4 ng/mL, or a PSA level greater than 3 ng/mL in men at increased risk of prostate cancer who have not undergone urological evaluation
- Elevated hematocrit greater than 48% (greater than 50% for those living at high altitude)
- Untreated severe obstructive sleep apnea
- Severe obstructive lower urinary tract symptoms
- Uncontrolled heart failure
- Myocardial infarction or stroke within the last 6 months
- Thrombophilia
- Those planning fertility in the near term
Initiating Testosterone Therapy
If the above criteria are met, and the patient and provider decide to initiate testosterone replacement therapy, the 2018 Endocrine Society Testosterone Therapy Guidelines recommend initiating testosterone replacement therapy using any of the suggested regimens based on personal preference, pharmacokinetics of the formulation, treatment burden, and cost. The FDA-approved testosterone replacement therapy options in the United States include intramuscular injection, transdermal gel, transdermal patch, an axillary solution, a buccal bioadhesive tablet, pellets, or a nasal gel.[155] Of note, testosterone is a controlled substance.
Monitoring After Initiation of Testosterone Replacement Therapy
- Monitoring to assess symptom response should take place 3 to 12 months after treatment initiation and then annually thereafter.
- Laboratory monitoring of testosterone concentrations should take place 3 to 6 months after initiation of testosterone replacement therapy, with the aim to achieve testosterone concentrations in the mid-normal range.
- Check hematocrit and hemoglobin levels 3 to 6 months after starting treatment and then annually.
- Monitor for prostate cancer risk during the first year after initiating testosterone replacement therapy (including checking a PSA level 3 to 12 months after starting testosterone and continuing with routine prostate cancer screening after 1 year).
Special Considerations in Persons with HIV
The interplay between testosterone deficiency and HIV is complex and has changed over the last several decades as a result of antiretroviral therapy. Available data suggest that men with HIV have a prevalence of testosterone deficiency that is roughly twice as high as in men without HIV.[157,158,159,160]
Screening Recommendations for Persons with HIV
The following summarizes the HIVMA/IDSA Primary Care Guidance recommendations for testosterone screening in persons with HIV.[16]
- Screening for testosterone deficiency in men with HIV should only be performed if the individual has symptoms of testosterone deficiency.
- The laboratory evaluation for testosterone deficiency should include a total testosterone level and a free testosterone level; the rationale for obtaining a free testosterone level is that HIV is associated with increased sex hormone binding globulin concentrations, which can lead to falsely elevated total testosterone levels.
- Blood samples to evaluate testosterone levels should be obtained in the morning, preferably before 10 a.m.
- All screening samples that are below the limit of normal should be confirmed with a repeat testosterone level.
- If an individual with HIV has low testosterone confirmed on two samples, measurement of LH and FSH should be performed to determine whether they have a primary (testicular) or central (pituitary or hypothalamic) cause for the testosterone deficiency.
Testosterone Replacement Therapy in Persons with HIV
The following summarizes HIVMA/IDSA Primary Care Guidance recommendations for testosterone replacement therapy in cisgender men with HIV.[16] The use of testosterone for gender-affirming masculinizing hormones is discussed in the section on Medical Care for Transgender Men in the lesson on HIV in Sexual and Gender Minority Populations.
- Indications to Start Testosterone Therapy: For cisgender men, testosterone replacement therapy should be prescribed with caution and only in those with symptomatic hypogonadism, given the potential long-term side effects that can occur with chronic testosterone use, particularly cardiac adverse effects.
- Testosterone Replacement Therapy: Persons with HIV should be treated with the same testosterone preparations and doses as in persons without HIV, as outlined above.
- Monitoring on Testosterone Therapy: Persons with HIV who are receiving testosterone replacement therapy should have the same monitoring as in persons without HIV, as outlined above.
Tobacco Use and Smoking Cessation
Overview
Tobacco use is a worldwide epidemic and is the leading preventable cause of death, disease, and disability in the United States. Data from the Centers for Disease Control and Prevention indicate that about 1 in 5 adults use tobacco products.[161] Tobacco use is a chronic disease and often requires behavioral support, pharmacologic therapy, and multiple attempts to quit. Tobacco use treatments are available and effective, and clinicians should be aware of best practices for counseling and treatment.
Guidelines for Tobacco Cessation
In 2008, the USPSTF released a clinical practice guideline for treating tobacco use and dependence.[162] This clinical guideline summarized the effectiveness of pharmacotherapy and concluded that certain pharmacotherapies are more effective than others, certain combinations are more effective than others, and the combination of counseling and medication is more effective than either alone (Figure 12).[162] In 2015 and 2021, the USPSTF released recommendations for Behavioral and Pharmacotherapy Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant People, and these recommendations were updated in 2021.[163,164] The USPSTF recommends that clinicians ask all adults about tobacco use, advise persons using tobacco to stop, and provide behavioral interventions and FDA-approved pharmacotherapies.[164] In 2018, the American College of Cardiology (ACC) published a decision pathway incorporating new evidence, for tobacco cessation treatment in adults; the following summarizes key points from the ACC recommendations.[165]
- The 5A’s: ask about tobacco use at every visit, advise all tobacco users to quit, assess willingness to quit, assist the individual in quitting (medications, counseling), and arrange follow-up contact.
- Telephonic tobacco quitlines may be able to provide intensive tobacco cessation counseling (1-800-QUITNOW). Intensive counseling has been proven more effective than brief intervention.
- Pharmacologic interventions should be offered as a component of smoking cessation programs. There are three main types of medications that have been shown to increase long-term smoking abstinence rates and are recommended for use in smoking cessation: varenicline, nicotine replacement products (gum, inhaler, lozenge, nasal spray, patch), and sustained-release bupropion (Table 6).
- Within 2 to 4 weeks of a quit attempt, follow-up contact with the individual attempting to quit is recommended, either in person or via telephone or electronic health record portal. This follow-up contact is important for monitoring tobacco cessation treatment, especially since the risk of smoking relapse is high in the immediate period after a quit attempt.
- Evidence regarding the use of electronic nicotine delivery systems (e-cigarettes, vaping) for tobacco cessation is insufficient to make recommendations.
- Evidence is also insufficient to assess the risks versus benefits of pharmacotherapy interventions for tobacco cessation in pregnant women.
Additional Pharmacologic Considerations
Despite early data that raised concerns about the cardiovascular safety of varenicline (and a warning on the package insert about this risk, especially in patients with known cardiovascular disease), a systematic review and meta-analysis concluded in 2016 that these concerns were unfounded; later that year, the FDA removed the varenicline black box warning.[165,166] After the release of the 2018 ACC guidelines, multiple reports have generated alarming concerns about the safety of vaping, and most experts would now advise extreme caution when considering electronic nicotine delivery systems.[167,168,169]
Special Considerations for Persons with HIV
Impact of Smoking in Persons with HIV
Individuals with HIV smoke at approximately twice the rate of those without HIV.[170,171] Among persons with HIV, one study in the United States found no difference in the prevalence of smoking in women versus men.[172] This finding contrasts with the overall United States population, where tobacco use is substantially higher among men than women.[173,174] Smoking is linked to multiple medical problems among individuals with HIV, including major cardiovascular disease, non-AIDS-defining cancers, and bacterial pneumonia.[175] In the HIV Outpatient Study, a prospective observational cohort study of persons with HIV receiving care since 1993, the attributable risk of incident cardiovascular disease events for tobacco smoking was 26.7%, which was similar to the attributable risk associated with baseline CD4 count less than 500 cells/mm3 and greater than the attributable risks associated with male sex or diabetes.[56]
Guidance for Smoking Cessation in Persons with HIV
The major tobacco cessation guidelines do not address smoking cessation in persons with HIV, and the HIVMA/IDSA Primary Care Guidance does not provide recommendations for specific interventions related to smoking cessation.[16,162,163,165] In a randomized, double-blind, placebo-controlled trial in France that involved 248 adults with HIV, investigators compared a 3-month course of varenicline in combination with smoking cessation counseling versus placebo with counseling.[176] At 48 weeks following the randomized intervention, a higher proportion of participants in the combination varenicline plus smoking cessation counseling arm had abstained from smoking as compared with the placebo-counseling arm.[176] There are no significant drug interactions between varenicline and antiretroviral therapy, though interactions can occur between bupropion and antiretroviral medications that may result in lower bupropion levels.[92]
Summary Points
- Cardiovascular diseases are an area of special concern to people with HIV, and cardiovascular risk reduction should be a priority.
- Hypertension in persons with HIV should be managed based on the same guidelines used for people without HIV, except that calcium channel blockers should be avoided with concomitant use of protease inhibitors or cobicistat.
- For people with HIV who are taking suppressive antiretroviral therapy and who would benefit from statin therapy, the preferred options are atorvastatin, rosuvastatin, and pitavastatin. Simvastatin and lovastatin should be avoided due to drug interactions with certain antiretroviral medications.
- People with HIV should undergo regular screening for the development of diabetes mellitus.
- People with HIV at increased risk for kidney disease should have routine laboratory monitoring of renal function. The risk of developing renal disease is higher for individuals with a CD4 count of less than 200 cells/mm3, elevated HIV RNA levels, Black race, female sex, older age, diabetes mellitus, and hypertension.
- Tenofovir DF carries a risk of nephrotoxicity in persons with HIV that is increased in persons with lower body weight, a lower creatinine clearance at tenofovir DF initiation, or receipt of a protease inhibitor boosted with ritonavir.
- All postmenopausal women and all men 50 years of age and older should receive DXA scans.
- Persons with HIV smoke at twice the rate of those without HIV, and persons with HIV who take antiretroviral therapy and who smoke lose more years of life to smoking than to HIV.
-
Among persons with HIV, Kaposi's sarcoma, non-Hodgkin’s lymphoma, and lung cancer are the most common cancers. Since 2003, the number of non-AIDS-defining cancers has exceeded the number of AIDS-defining cancers.
- Colon cancer, breast cancer, and prostate cancer screening recommendations are the same for persons with HIV as for the general population. Due to disproportional risks of developing cervical and anal cancer among individuals with HIV, these cancers warrant different screening protocols.
Citations
- 1.Palella FJ Jr, Baker RK, Moorman AC, et al. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43:27-34.[PubMed Abstract] -
- 2.Patel P, Hanson DL, Sullivan PS, et al. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992-2003. Ann Intern Med. 2008;148:728-36.[PubMed Abstract] -
- 3.Pantanowitz L, Dezube BJ. Evolving spectrum and incidence of non-AIDS-defining malignancies. Curr Opin HIV AIDS. 2009;4:27-34.[PubMed Abstract] -
- 4.Shiels MS, Islam JY, Rosenberg PS, Hall HI, Jacobson E, Engels EA. Projected Cancer Incidence Rates and Burden of Incident Cancer Cases in HIV-Infected Adults in the United States Through 2030. Ann Intern Med. 2018;168:866-73.[PubMed Abstract] -
- 5.Ingle SM, May MT, Gill MJ, et al. Impact of risk factors for specific causes of death in the first and subsequent years of antiretroviral therapy among HIV-infected patients. Clin Infect Dis. 2014;59:287-97.[PubMed Abstract] -
- 6.Silverberg MJ, Neuhaus J, Bower M, et al. Risk of cancers during interrupted antiretroviral therapy in the SMART study. AIDS. 2007;21:1957-63.[PubMed Abstract] -
- 7.Hernández-Ramírez RU, Shiels MS, Dubrow R, Engels EA. Cancer risk in HIV-infected people in the USA from 1996 to 2012: a population-based, registry-linkage study. Lancet HIV. 2017;4:e495-e504.[PubMed Abstract] -
- 8.Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst. 2011;103:753-62.[PubMed Abstract] -
- 9.Engels EA, Biggar RJ, Hall HI, et al. Cancer risk in people infected with human immunodeficiency virus in the United States. Int J Cancer. 2008;123:187-94.[PubMed Abstract] -
- 10.Centers for Disease Control and Prevention. HIV Surveillance Report, 2005;vol.17. Published 2007.[CDC] -
- 11.Robbins HA, Pfeiffer RM, Shiels MS, Li J, Hall HI, Engels EA. Excess cancers among HIV-infected people in the United States. J Natl Cancer Inst. 2015;107:.[PubMed Abstract] -
- 12.de Martel C, Shiels MS, Franceschi S, et al. Cancers attributable to infections among adults with HIV in the United States. AIDS. 2015;29:2173-81.[PubMed Abstract] -
- 13.Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370:59-67.[PubMed Abstract] -
- 14.U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2021 submission data (1999-2019): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute.
- 15.Voutsadakis IA, Silverman LR. Breast cancer in HIV-positive women: a report of four cases and review of the literature. Cancer Invest. 2002;20:452-7.[PubMed Abstract] -
- 16.Thompson MA, Horberg MA, Agwu AL, et al. Primary Care Guidance for Persons With Human Immunodeficiency Virus: 2020 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2021;73:e3572-e3605[HIVMA] -
- 17.US Preventive Services Task Force; Nicholson WK, Silverstein M, et al. Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2024;331:1918-30.[PubMed Abstract] -
- 18.Oeffinger KC, Fontham ET, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update From the American Cancer Society. JAMA. 2015;314:1599-614.[PubMed Abstract] -
- 19.Myers ER, Moorman P, Gierisch JM, et al. Benefits and Harms of Breast Cancer Screening: A Systematic Review. JAMA. 2015;314:1615-34.[PubMed Abstract] -
- 20.Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145-64.[PubMed Abstract] -
- 21.Davidson KW, Barry MJ, Mangione CM, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:1965-77.[PubMed Abstract] -
- 22.Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250-281.[PubMed Abstract] -
- 23.Patel SG, May FP, Anderson JC, et al. Updates on Age to Start and Stop Colorectal Cancer Screening: Recommendations From the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2022;117:57-69.[PubMed Abstract] -
- 24.Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307-23.[PubMed Abstract] -
- 25.Gupta S, Lieberman D, Anderson JC, et al. Recommendations for Follow-Up After Colonoscopy and Polypectomy: A Consensus Update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2020;158:1131-53.e5.[PubMed Abstract] -
- 26.Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872-85.[PubMed Abstract] -
- 27.Moyer VA. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:330-8.[PubMed Abstract] -
- 28.US Preventive Services Task Force, Krist AH, Davidson KW, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:962-70.[PubMed Abstract] -
- 29.Sigel K, Makinson A, Thaler J. Lung cancer in persons with HIV. Curr Opin HIV AIDS. 2017;12:31-38.[PubMed Abstract] -
- 30.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409.[PubMed Abstract] -
- 31.Pinsky PF, Church TR, Izmirlian G, Kramer BS. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Cancer. 2013;119:3976-83.[PubMed Abstract] -
- 32.Marcus JL, Chao CR, Leyden WA, et al. Prostate cancer incidence and prostate-specific antigen testing among HIV-positive and HIV-negative men. J Acquir Immune Defic Syndr. 2014;66:495-502.[PubMed Abstract] -
- 33.US Preventive Services Task Force, Grossman DC, Curry SJ, et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319:1901-1913.[PubMed Abstract] -
- 34.Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024.[HIV.gov] -
- 35.Colón-López V, Shiels MS, Machin M, et al. Anal Cancer Risk Among People With HIV Infection in the United States. J Clin Oncol. 2018;36:68-75.[PubMed Abstract] -
- 36.Clifford GM, Georges D, Shiels MS, et al. A meta-analysis of anal cancer incidence by risk group: Toward a unified anal cancer risk scale. Int J Cancer. 2021;148:38-47.[PubMed Abstract] -
- 37.Palefsky JM, Lee JY, Jay N, et al. Treatment of Anal High-Grade Squamous Intraepithelial Lesions to Prevent Anal Cancer. N Engl J Med. 2022;386:2273-82.[PubMed Abstract] -
- 38.ASCEND Study Collaborative Group, Bowman L, Mafham M, et al. Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. N Engl J Med. 2018;379:1529-39.[PubMed Abstract] -
- 39.Gaziano JM, Brotons C, Coppolecchia R, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392:1036-46.[PubMed Abstract] -
- 40.McNeil JJ, Nelson MR, Woods RL, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med. 2018;379:1519-28.[PubMed Abstract] -
- 41.Knickelbine T, Miedema MD. Aspirin for primary prevention of cardiovascular disease: is it time to move on? Curr Opin Cardiol. 2019;34:510-13.[PubMed Abstract] -
- 42.US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement. JAMA. 2022;327:1577-84.[PubMed Abstract] -
- 43.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:e177-e232.[PubMed Abstract] -
- 44.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:1376-1414.[PubMed Abstract] -
- 45.ElSayed NA, Aleppo G, Aroda VR, et al. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S158-S190.[PubMed Abstract] -
- 46.Zucker EJ, Misono AS, Prabhakar AM. Abdominal Aortic Aneurysm Screening Practices: Impact of the 2014 U.S. Preventive Services Task Force Recommendations. J Am Coll Radiol. 2017;14:868-74.[PubMed Abstract] -
- 47.Tang W, Yao L, Roetker NS, et al. Lifetime Risk and Risk Factors for Abdominal Aortic Aneurysm in a 24-Year Prospective Study: The ARIC Study (Atherosclerosis Risk in Communities). Arterioscler Thromb Vasc Biol. 2016 Dec;36:2468-77.[PubMed Abstract] -
- 48.Owens DK, Davidson KW, Krist AH, et al. Screening for Abdominal Aortic Aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:2211-8.[PubMed Abstract] -
- 49.Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614-22.[PubMed Abstract] -
- 50.Grinspoon SK. Cardiovascular Disease in HIV: Traditional and Nontraditional Risk Factors. Top Antivir Med. 2014;22:676-679.[PubMed Abstract] -
- 51.Klein D, Hurley LB, Quesenberry CP Jr, Sidney S. Do protease inhibitors increase the risk for coronary heart disease in patients with HIV-1 infection? J Acquir Immune Defic Syndr. 2002;30:471-7.[PubMed Abstract] -
- 52.Shah ASV, Stelzle D, Lee KK, et al. Global Burden of Atherosclerotic Cardiovascular Disease in People Living With HIV. Circulation. 2018;138:1100-12.[PubMed Abstract] -
- 53.Feinstein MJ, Hsue PY, Benjamin LA, et al. Characteristics, Prevention, and Management of Cardiovascular Disease in People Living With HIV: A Scientific Statement From the American Heart Association. Circulation. 2019;140:e98-e124.[PubMed Abstract] -
- 54.Bozzette SA. HIV and Cardiovascular Disease. Clin Infect Dis. 2011;53:92-3.[PubMed Abstract] -
- 55.Dubé MP, Wu JW, Aberg JA, et al. Safety and efficacy of extended-release niacin for the treatment of dyslipidaemia in patients with HIV infection: AIDS Clinical Trials Group Study A5148. Antivir Ther. 2006;11:1081-9.[PubMed Abstract] -
- 56.Lichtenstein KA, Armon C, Buchacz K, et al. Low CD4+ T cell count is a risk factor for cardiovascular disease events in the HIV outpatient study. Clin Infect Dis. 2010;51:435-47.[PubMed Abstract] -
- 57.Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab. 2007;92:2506-12.[PubMed Abstract] -
- 58.El-Sadr WM, Lundgren J, Neaton JD, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283-96.[PubMed Abstract] -
- 59.SMART/INSIGHT; DAD Study Groups. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients. AIDS. 2008;22:F17-24.[PubMed Abstract] -
- 60.Obel N, Farkas DK, Kronborg G, et al. Abacavir and risk of myocardial infarction in HIV-infected patients on highly active antiretroviral therapy: a population-based nationwide cohort study. HIV Med. 2010;11:130-6.[PubMed Abstract] -
- 61.Durand M, Sheehy O, Baril JG, Lelorier J, Tremblay CL. Association between HIV infection, antiretroviral therapy, and risk of acute myocardial infarction: a cohort and nested case-control study using Québec's public health insurance database. J Acquir Immune Defic Syndr. 2011;57:245-53.[PubMed Abstract] -
- 62.Ding X, Andraca-Carrera E, Cooper C, et al. No association of abacavir use with myocardial infarction: findings of an FDA meta-analysis. J Acquir Immune Defic Syndr. 2012;61:441-7.[PubMed Abstract] -
- 63.Sabin CA, Worm SW, Weber R, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet. 2008;371:1417-26.[PubMed Abstract] -
- 64.Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) study. J Infect Dis. 2010;201:318-30.[PubMed Abstract] -
- 65.Monforte Ad, Reiss P, Ryom L, et al. Atazanavir is not associated with an increased risk of cardio- or cerebrovascular disease events. AIDS. 2013;27:407-15.[PubMed Abstract] -
- 66.Hsue PY, Waters DD. HIV infection and coronary heart disease: mechanisms and management. Nat Rev Cardiol. 2019;16:745-759.[PubMed Abstract] -
- 67.So-Armah K, Benjamin LA, Bloomfield GS, et al. HIV and cardiovascular disease. Lancet HIV. 2020;7:e279-e293.[PubMed Abstract] -
- 68.Filipkowski AM, Kundu S, Eden SK, et al. Association of HIV Infection and Incident Abdominal Aortic Aneurysm Among 143 001 Veterans. Circulation. 2023 May 25. [Online Ahead of Print][PubMed Abstract] -
- 69.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153-e639.[PubMed Abstract] -
- 70.ElSayed NA, Aleppo G, Aroda VR, et al. 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S203-S215.[PubMed Abstract] -
- 71.ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S140-S157.[PubMed Abstract] -
- 72.ElSayed NA, Aleppo G, Aroda VR, et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S128-S139.[PubMed Abstract] -
- 73.ElSayed NA, Aleppo G, Aroda VR, et al. 6. Glycemic Targets: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S97-S110.[PubMed Abstract] -
- 74.ElSayed NA, Aleppo G, Aroda VR, et al. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S49-S67.[PubMed Abstract] -
- 75.ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S19-S40.[PubMed Abstract] -
- 76.ElSayed NA, Aleppo G, Aroda VR, et al. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S10-S18.[PubMed Abstract] -
- 77.ElSayed NA, Aleppo G, Aroda VR, et al. 3. Prevention or Delay of Type 2 Diabetes and Associated Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S41-S48.[PubMed Abstract] -
- 78.ElSayed NA, Aleppo G, Aroda VR, et al. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S68-S96.[PubMed Abstract] -
- 79.ElSayed NA, Aleppo G, Aroda VR, et al. 7. Diabetes Technology: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S111-S127.[PubMed Abstract] -
- 80.Zoungas S, Chalmers J, Neal B, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371:1392-406.[PubMed Abstract] -
- 81.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143.[PubMed Abstract] -
- 82.Monroe AK, Glesby MJ, Brown TT. Diagnosing and managing diabetes in HIV-infected patients: current concepts. Clin Infect Dis. 2015;60:453-62.[PubMed Abstract] -
- 83.Lucas GM, Ross MJ, Stock PG, et al. Clinical Practice Guideline for the Management of Chronic Kidney Disease in Patients Infected With HIV: 2014 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96-e138.[PubMed Abstract] -
- 84.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions. Table 24d. Drug interactions between integrase strand transfer inhibitors and other drugs. September 12, 2024.[HIV.gov] -
- 85.National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey (NHANES). Fact Sheet. July 2020.
- 86.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269.[PubMed Abstract] -
- 87.Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982-1004.[PubMed Abstract] -
- 88.Nüesch R, Wang Q, Elzi L, et al. Risk of cardiovascular events and blood pressure control in hypertensive HIV-infected patients: Swiss HIV Cohort Study (SHCS). J Acquir Immune Defic Syndr. 2013;62:396-404.[PubMed Abstract] -
- 89.Armah KA, Chang CC, Baker JV, et al. Prehypertension, hypertension, and the risk of acute myocardial infarction in HIV-infected and -uninfected veterans. Clin Infect Dis. 2013;58:121-9.[PubMed Abstract] -
- 90.Krauskopf K, Van Natta ML, Danis RP, et al. Correlates of hypertension in patients with AIDS in the era of highly active antiretroviral therapy. J Int Assoc Provid AIDS Care. 2013;12:325-33.[PubMed Abstract] -
- 91.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug interactions. Table 24a. Drug interactions between protease inhibitors and other drugs. September 1, 2022.[HIV.gov] -
- 92.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Drug-drug Interactions: overview. May 26, 2023.[HIV.gov] -
- 93.Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med. 2015;372:2387-97.[PubMed Abstract] -
- 94.Morrone D, Weintraub WS, Toth PP, et al. Lipid-altering efficacy of ezetimibe plus statin and statin monotherapy and identification of factors associated with treatment response: a pooled analysis of over 21,000 subjects from 27 clinical trials. Atherosclerosis. 2012;223:251-61.[PubMed Abstract] -
- 95.Rosenson RS, Hegele RA, Fazio S, Cannon CP. The Evolving Future of PCSK9 Inhibitors. J Am Coll Cardiol. 2018;72:314-329.[PubMed Abstract] -
- 96.Bergeron N, Phan BA, Ding Y, Fong A, Krauss RM. Proprotein convertase subtilisin/kexin type 9 inhibition: a new therapeutic mechanism for reducing cardiovascular disease risk. Circulation. 2015;132:1648-66.[PubMed Abstract] -
- 97.Burnett JR, Hooper AJ. PCSK9 - A Journey to Cardiovascular Outcomes. N Engl J Med. 2018;379:2161-2.[PubMed Abstract] -
- 98.Kazi DS, Penko J, Coxson PG, Guzman D, Wei PC, Bibbins-Domingo K. Cost-Effectiveness of Alirocumab: A Just-in-Time Analysis Based on the ODYSSEY Outcomes Trial. Ann Intern Med. 2019;170:221-229.[PubMed Abstract] -
- 99.Rader DJ, Haffner SM. Role of fibrates in the management of hypertriglyceridemia. Am J Cardiol. 1999;83:30F-35F.[PubMed Abstract] -
- 100.Schoonjans K, Staels B, Auwerx J. Role of the peroxisome proliferator-activated receptor (PPAR) in mediating the effects of fibrates and fatty acids on gene expression. J Lipid Res. 1996;37:907-25.[PubMed Abstract] -
- 101.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;129(25 Suppl 2):S46-8.[PubMed Abstract] -
- 102.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. Department of Health and Human Services. Statin Therapy in People with HIV. February 27, 2024[HIV.gov] -
- 103.Grinspoon SK, Fitch KV, Zanni MV, et al. Pitavastatin to Prevent Cardiovascular Disease in HIV Infection. N Engl J Med. 2023;389:687-99.[PubMed Abstract] -
- 104.Zanni MV, Toribio M, Robbins GK, et al. Effects of Antiretroviral Therapy on Immune Function and Arterial Inflammation in Treatment-Naive Patients With Human Immunodeficiency Virus Infection. JAMA Cardiol. 2016;1:474-80.[PubMed Abstract] -
- 105.Dubé MP, Stein JH, Aberg JA, et al. Guidelines for the evaluation and management of dyslipidemia in human immunodeficiency virus (HIV)-infected adults receiving antiretroviral therapy: recommendations of the HIV Medical Association of the Infectious Disease Society of America and the Adult AIDS Clinical Trials Group. Clin Infect Dis. 2003;37:613-27.[PubMed Abstract] -
- 106.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Limitations to treatment safety and efficacy: adverse effects of antiretroviral agents. May 26, 2023.[HIV.gov] -
- 107.Eron JJ, Young B, Cooper DA, et al. Switch to a raltegravir-based regimen versus continuation of a lopinavir-ritonavir-based regimen in stable HIV-infected patients with suppressed viraemia (SWITCHMRK 1 and 2): two multicentre, double-blind, randomised controlled trials. Lancet. 2010;375:396-407.[PubMed Abstract] -
- 108.Gatell J, Salmon-Ceron D, Lazzarin A, et al. Efficacy and safety of atazanavir-based highly active antiretroviral therapy in patients with virologic suppression switched from a stable, boosted or unboosted protease inhibitor treatment regimen: the SWAN Study (AI424-097) 48-week results. Clin Infect Dis. 2007;44:1484-92.[PubMed Abstract] -
- 109.Tungsiripat M, Kitch D, Glesby MJ, et al. A pilot study to determine the impact on dyslipidemia of adding tenofovir to stable background antiretroviral therapy: ACTG 5206. AIDS. 2010;24:1781-4.[PubMed Abstract] -
- 110.Malvestutto CD, Aberg JA. Management of dyslipidemia in HIV-infected patients. Clin Lipidol. 2011;6:447-462.[PubMed Abstract] -
- 111.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Department of Health and Human Services. Laboratory testing: laboratory testing for initial assessment and monitoring of people with HIV receiving antiretroviral therapy. September 21, 2022.[HIV.gov] -
- 112.Keaney JF Jr, Curfman GD, Jarcho JA. A pragmatic view of the new cholesterol treatment guidelines. N Engl J Med. 2014;370:275-8.[PubMed Abstract] -
- 113.Mallolas J, Podzamczer D, Milinkovic A, et al. Efficacy and safety of switching from boosted lopinavir to boosted atazanavir in patients with virological suppression receiving a LPV/r-containing HAART: the ATAZIP study. J Acquir Immune Defic Syndr. 2009;51:29-36.[PubMed Abstract] -
- 114.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. Department of Health and Human Services. Drug-drug interactions. Table 24b. Drug interactions between non-nucleoside reverse transcriptase inhibitors and other drugs. September 1, 2022[HIV.gov] -
- 115.Leyes P, Martínez E, Larrousse M, et al. Effects of ezetimibe on cholesterol metabolism in HIV-infected patients with protease inhibitor-associated dyslipidemia: a single-arm intervention trial. BMC Infect Dis. 2014;14:497.[PubMed Abstract] -
- 116.Saeedi R, Johns K, Frohlich J, Bennett MT, Bondy G. Lipid lowering efficacy and safety of Ezetimibe combined with rosuvastatin compared with titrating rosuvastatin monotherapy in HIV-positive patients. Lipids Health Dis. 2015;14:57.[PubMed Abstract] -
- 117.Wohl DA, Waters D, Simpson RJ Jr, et al. Ezetimibe alone reduces low-density lipoprotein cholesterol in HIV-infected patients receiving combination antiretroviral therapy. Clin Infect Dis. 2008;47:1105-8.[PubMed Abstract] -
- 118.Kotler DP. HIV and antiretroviral therapy: lipid abnormalities and associated cardiovascular risk in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;49 Suppl 2:S79-85.[PubMed Abstract] -
- 119.Worm SW, Kamara DA, Reiss P, et al. Elevated triglycerides and risk of myocardial infarction in HIV-positive persons. AIDS. 2011;25:1497-504.[PubMed Abstract] -
- 120.US Preventive Services Task Force, Curry SJ, Krist AH, et al. Screening for Osteoporosis to Prevent Fractures: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319:2521-2531.[PubMed Abstract] -
- 121.Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25:2359-81.[PubMed Abstract] -
- 122.Qaseem A, Forciea MA, McLean RM, Denberg TD. Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women: A Clinical Practice Guideline Update From the American College of Physicians. Ann Intern Med. 2017;166:818-839.[PubMed Abstract] -
- 123.Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520-6.[PubMed Abstract] -
- 124.Schwartz AV, Bauer DC, Cummings SR, et al. Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res. 2010;25:976-82.[PubMed Abstract] -
- 125.Whitaker M, Guo J, Kehoe T, Benson G. Bisphosphonates for osteoporosis--where do we go from here? N Engl J Med. 2012;366:2048-51.[PubMed Abstract] -
- 126.McComsey GA, Tebas P, Shane E, et al. Bone disease in HIV infection: a practical review and recommendations for HIV care providers. Clin Infect Dis. 2010;51:937-46.[PubMed Abstract] -
- 127.Mascarau R, Bertrand F, Labrousse A, et al. HIV-1-Infected Human Macrophages, by Secreting RANK-L, Contribute to Enhanced Osteoclast Recruitment. Int J Mol Sci. 2020;21:3154.[PubMed Abstract] -
- 128.Brown TT, Hoy J, Borderi M, et al. Recommendations for Evaluation and Management of Bone Disease in HIV. Clin Infect Dis. 2015;60:1242-51.[PubMed Abstract] -
- 129.McComsey GA, Kitch D, Daar ES, et al. Bone mineral density and fractures in antiretroviral-naive persons randomized to receive abacavir-lamivudine or tenofovir disoproxil fumarate-emtricitabine along with efavirenz or atazanavir-ritonavir: Aids Clinical Trials Group A5224s, a substudy of ACTG A5202. J Infect Dis. 2011;203:1791-801.[PubMed Abstract] -
- 130.Mills A, Arribas JR, Andrade-Villanueva J, et al. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in antiretroviral regimens for virologically suppressed adults with HIV-1 infection: a randomised, active-controlled, multicentre, open-label, phase 3, non-inferiority study. Lancet Infect Dis. 2016;16:43-52.[PubMed Abstract] -
- 131.Sax PE, Wohl D, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomised, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606-15.[PubMed Abstract] -
- 132.Migliorati CA, Siegel MA, Elting LS. Bisphosphonate-associated osteonecrosis: a long-term complication of bisphosphonate treatment. Lancet Oncol. 2006;7:508-14.[PubMed Abstract] -
- 133.Saita Y, Ishijima M, Kaneko K. Atypical femoral fractures and bisphosphonate use: current evidence and clinical implications. Ther Adv Chronic Dis. 2015;6:185-93.[PubMed Abstract] -
- 134.Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713-35.[PubMed Abstract] -
- 135.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1-266.[PubMed Abstract] -
- 136.Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137-47.[PubMed Abstract] -
- 137.Cohen SD, Kopp JB, Kimmel PL. Kidney Diseases Associated with Human Immunodeficiency Virus Infection. N Engl J Med. 2017;377:2363-74.[PubMed Abstract] -
- 138.Mallipattu SK, Salem F, Wyatt CM. The changing epidemiology of HIV-related chronic kidney disease in the era of antiretroviral therapy. Kidney Int. 2014;86:259-65.[PubMed Abstract] -
- 139.Scherzer R, Estrella M, Li Y, et al. Association of tenofovir exposure with kidney disease risk in HIV infection. AIDS. 2012;26:867-75.[PubMed Abstract] -
- 140.Mocroft A, Kirk O, Reiss P, et al. Estimated glomerular filtration rate, chronic kidney disease and antiretroviral drug use in HIV-positive patients. AIDS. 2010;24:1667-78.[PubMed Abstract] -
- 141.Cooper RD, Wiebe N, Smith N, Keiser P, Naicker S, Tonelli M. Systematic review and meta-analysis: renal safety of tenofovir disoproxil fumarate in HIV-infected patients. Clin Infect Dis. 2010;51:496-505.[PubMed Abstract] -
- 142.Gupta SK, Anderson AM, Ebrahimi R, et al. Fanconi syndrome accompanied by renal function decline with tenofovir disoproxil fumarate: a prospective, case-control study of predictors and resolution in HIV-infected patients. PLoS One. 2014;9:e92717.[PubMed Abstract] -
- 143.Hamzah L, Williams D, Bailey AC, et al. Early safety of tenofovir alafenamide in patients with a history of tubulopathy on tenofovir disoproxil fumarate: a randomized controlled clinical trial. HIV Med. 2020;21:198-203.[PubMed Abstract] -
- 144.Bahr NC, Yarlagadda SG. Fanconi Syndrome and Tenofovir Alafenamide: A Case Report. Ann Intern Med. 2019;170:814-815.[PubMed Abstract] -
- 145.Novick TK, Choi MJ, Rosenberg AZ, McMahon BA, Fine D, Atta MG. Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.[PubMed Abstract] -
- 146.Serota DP, Franch HA, Cartwright EJ. Acute Kidney Injury in a Patient on Tenofovir Alafenamide Fumarate After Initiation of Treatment for Hepatitis C Virus Infection. Open Forum Infect Dis. 2018;5:ofy189.[PubMed Abstract] -
- 147.German P, Liu HC, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.[PubMed Abstract] -
- 148.Lindeman TA, Duggan JM, Sahloff EG. Evaluation of Serum Creatinine Changes With Integrase Inhibitor Use in Human Immunodeficiency Virus-1 Infected Adults. Open Forum Infect Dis. 2016;3:ofw053.[PubMed Abstract] -
- 149.Jones CY, Jones CA, Wilson IB, et al. Cystatin C and creatinine in an HIV cohort: the nutrition for healthy living study. Am J Kidney Dis. 2008;51:914-24.[PubMed Abstract] -
- 150.Odden MC, Scherzer R, Bacchetti P, et al. Cystatin C level as a marker of kidney function in human immunodeficiency virus infection: the FRAM study. Arch Intern Med. 2007;167:2213-9.[PubMed Abstract] -
- 151.Gagneux-Brunon A, Mariat C, Delanaye P. Cystatin C in HIV-infected patients: promising but not yet ready for prime time. Nephrol Dial Transplant. 2012;27:1305-13.[PubMed Abstract] -
- 152.Weiner DE, Tighiouart H, Amin MG, et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol. 2004;15:1307-15.[PubMed Abstract] -
- 153.Longenecker CT, Hileman CO, Funderburg NT, McComsey GA. Rosuvastatin preserves renal function and lowers cystatin C in HIV-infected subjects on antiretroviral therapy: the SATURN-HIV trial. Clin Infect Dis. 2014;59:1148-56.[PubMed Abstract] -
- 154.Layton JB, Li D, Meier CR, et al. Testosterone lab testing and initiation in the United Kingdom and the United States, 2000 to 2011. J Clin Endocrinol Metab. 2014;99:835-42.[PubMed Abstract] -
- 155.Bhasin S, Brito JP, Cunningham GR, et al. Testosterone Therapy in Men With Hypogonadism: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2018;103:1715-1744.[PubMed Abstract] -
- 156.Vigen R, O'Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310:1829-36.[PubMed Abstract] -
- 157.Dobs AS, Dempsey MA, Ladenson PW, Polk BF. Endocrine disorders in men infected with human immunodeficiency virus. Am J Med. 1988;84:611-6.[PubMed Abstract] -
- 158.Gomes AR, Souteiro P, Silva CG, et al. Prevalence of testosterone deficiency in HIV-infected men under antiretroviral therapy. BMC Infect Dis. 2016;16:628.[PubMed Abstract] -
- 159.Lachâtre M, Pasquet A, Ajana F, et al. HIV and hypogonadism: a new challenge for young-aged and middle-aged men on effective antiretroviral therapy. AIDS. 2017;31:451-3.[PubMed Abstract] -
- 160.Bhatia R, Murphy AB, Raper JL, et al. Testosterone replacement therapy among HIV-infected men in the CFAR Network of Integrated Clinical Systems. AIDS. 2015;29:77-81.[PubMed Abstract] -
- 161.Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69:1736-42.[PubMed Abstract] -
- 162.U.S. Public Health Service. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158-76.[PubMed Abstract] -
- 163.Siu AL. Behavioral and Pharmacotherapy Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Women: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163:622-34.[PubMed Abstract] -
- 164.US Preventive Services Task Force; Krist AH, Davidson KW, et al. Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Persons: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:265-79.[PubMed Abstract] -
- 165.Barua RS, Rigotti NA, Benowitz NL, et al. 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2018;72:3332-65.[PubMed Abstract] -
- 166.Sterling LH, Windle SB, Filion KB, Touma L, Eisenberg MJ. Varenicline and Adverse Cardiovascular Events: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2016;5(2).[PubMed Abstract] -
- 167.Butt YM, Smith ML, Tazelaar HD, et al. Pathology of Vaping-Associated Lung Injury. N Engl J Med. 2019;381:1780-1.[PubMed Abstract] -
- 168.Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Final Report. N Engl J Med. 2020;382:903-16.[PubMed Abstract] -
- 169.Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary Lipid-Laden Macrophages and Vaping. N Engl J Med. 2019;381:1488-9.[PubMed Abstract] -
- 170.Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162:335-44.[PubMed Abstract] -
- 171.Frazier EL, Sutton MY, Brooks JT, Shouse RL, Weiser J. Trends in cigarette smoking among adults with HIV compared with the general adult population, United States - 2009-2014. Prev Med. 2018;111:231-4.[PubMed Abstract] -
- 172.Weinberger AH, Smith PH, Funk AP, Rabin S, Shuter J. Sex Differences in Tobacco Use Among Persons Living With HIV/AIDS: A Systematic Review and Meta-Analysis. J Acquir Immune Defic Syndr. 2017;74:439-453.[PubMed Abstract] -
- 173.Elf JL, Variava E, Chon S, et al. Prevalence and Correlates of Smoking Among People Living With HIV in South Africa. Nicotine Tob Res. 2018;20:1124-31.[PubMed Abstract] -
- 174.Mdege ND, Shah S, Ayo-Yusuf OA, Hakim J, Siddiqi K. Tobacco use among people living with HIV: analysis of data from Demographic and Health Surveys from 28 low-income and middle-income countries. Lancet Glob Health. 2017;5:e578-e592.[PubMed Abstract] -
- 175.Lifson AR, Neuhaus J, Arribas JR, van den Berg-Wolf M, Labriola AM, Read TR. Smoking-related health risks among persons with HIV in the Strategies for Management of Antiretroviral Therapy clinical trial. Am J Public Health. 2010;100:1896-903.[PubMed Abstract] -
- 176.Mercié P, Arsandaux J, Katlama C, et al. Efficacy and safety of varenicline for smoking cessation in people living with HIV in France (ANRS 144 Inter-ACTIV): a randomised controlled phase 3 clinical trial. Lancet HIV. 2018;5:e126-e135.[PubMed Abstract] -
Additional References
- Albright ES, Ovalle F, Bell DS. Artificially low hemoglobin A1c caused by use of dapsone. Endocr Pract. 2002;8:370-2.[PubMed Abstract] -
- Anal Cancer HSIL Outcomes Research (ANCHOR) Study.[ANCHOR Study] -
- Armah KA, Chang CC, Baker JV, et al. Prehypertension, hypertension, and the risk of acute myocardial infarction in HIV-infected and -uninfected veterans. Clin Infect Dis. 2013;58:121-9.[PubMed Abstract] -
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146-e603.[PubMed Abstract] -
- Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56-e528.[PubMed Abstract] -
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67-e492.[PubMed Abstract] -
- Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536-59.[PubMed Abstract] -
- Bibbins-Domingo K. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164:836-45.[PubMed Abstract] -
- Boyd SD, Hadigan C, McManus M, et al. Influence of low-dose ritonavir with and without darunavir on the pharmacokinetics and pharmacodynamics of inhaled beclomethasone. J Acquir Immune Defic Syndr. 2013;63:355-61.[PubMed Abstract] -
- Brown TT, Cole SR, Li X, et al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. 2005;165:1179-84.[PubMed Abstract] -
- Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev. 2013:CD009329.[PubMed Abstract] -
- Cattelan AM, Trevenzoli M, Sasset L, Rinaldi L, Balasso V, Cadrobbi P. Indinavir and systemic hypertension. AIDS. 2001;15:805-7.[PubMed Abstract] -
- Centers for Disease and Prevention. Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol--United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60:109-14.[MMWR] -
- Cheng J, Zhang W, Zhang X, et al. Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis. JAMA Intern Med. 2014;174:773-85.[PubMed Abstract] -
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-72.[PubMed Abstract] -
- Chow DC, Souza SA, Chen R, Richmond-Crum SM, Grandinetti A, Shikuma C. Elevated blood pressure in HIV-infected individuals receiving highly active antiretroviral therapy. HIV Clin Trials. 2003;4:411-6.[PubMed Abstract] -
- Coelho AR, Moreira FA, Santos AC, et al. Diabetes mellitus in HIV-infected patients: fasting glucose, A1c, or oral glucose tolerance test - which method to choose for the diagnosis? BMC Infect Dis. 2018;18:309.[PubMed Abstract] -
- Coghill AE, Shiels MS, Suneja G, Engels EA. Elevated Cancer-Specific Mortality Among HIV-Infected Patients in the United States. J Clin Oncol. 2015;33:2376-83.[PubMed Abstract] -
- Cotter AG, Sabin CA, Simelane S, et al. Relative contribution of HIV infection, demographics and body mass index to bone mineral density. AIDS. 2014;28:2051-60.[PubMed Abstract] -
- Cruciani M, Zanichelli V, Serpelloni G, et al. Abacavir use and cardiovascular disease events: a meta-analysis of published and unpublished data. AIDS. 2011;25:1993-2004.[PubMed Abstract] -
- Davidson KW, Barry MJ, Mangione CM, et al. Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:736-43.[PubMed Abstract] -
- Diop ME, Bastard JP, Meunier N, et al. Inappropriately low glycated hemoglobin values and hemolysis in HIV-infected patients. AIDS Res Hum Retroviruses. 2006;22:1242-7.[PubMed Abstract] -
- Ebbert JO, Hatsukami DK, Croghan IT, et al. Combination varenicline and bupropion SR for tobacco-dependence treatment in cigarette smokers: a randomized trial. JAMA. 2014;311:155-63.[PubMed Abstract] -
- Eckhardt BJ, Holzman RS, Kwan CK, Baghdadi J, Aberg JA. Glycated Hemoglobin A(1c) as screening for diabetes mellitus in HIV-infected individuals. AIDS Patient Care STDS. 2012;26:197-201.[PubMed Abstract] -
- ElSayed NA, Aleppo G, Aroda VR, et al. 11. Chronic Kidney Disease and Risk Management: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S191-S202.[PubMed Abstract] -
- Erlandson KM, Jiang Y, Debanne SM, McComsey GA. Effects of 96 Weeks of Rosuvastatin on Bone, Muscle, and Fat in HIV-Infected Adults on Effective Antiretroviral Therapy. AIDS Res Hum Retroviruses. 2016;32:311-6.[PubMed Abstract] -
- Erlandson KM, Jiang Y, Debanne SM, McComsey GA. Effects of randomized rosuvastatin compared with placebo on bone and body composition among HIV-infected adults. AIDS. 2015;29:175-82.[PubMed Abstract] -
- Feinstein MJ, Achenbach CJ, Stone NJ, Lloyd-Jones DM. A Systematic Review of the Usefulness of Statin Therapy in HIV-Infected Patients. Am J Cardiol. 2015; pii: S0002-9149(15)00980-7.[PubMed Abstract] -
- Feldman JG, Minkoff H, Schneider MF, et al. Association of cigarette smoking with HIV prognosis among women in the HAART era: a report from the women's interagency HIV study. Am J Public Health. 2006;96:1060-5.[PubMed Abstract] -
- Fichtenbaum CJ, Yeh TM, Evans SR, Aberg JA. Treatment with pravastatin and fenofibrate improves atherogenic lipid profiles but not inflammatory markers in ACTG 5087. J Clin Lipidol. 2010;4:279-87.[PubMed Abstract] -
- Galli L, Spagnuolo V, Poli A, et al. Use of statins and risk of AIDS-defining and non-AIDS-defining malignancies among HIV-1 infected patients on antiretroviral therapy. AIDS. 2014;28:2407-15.[PubMed Abstract] -
- Gerber JG, Kitch DW, Fichtenbaum CJ, et al. Fish oil and fenofibrate for the treatment of hypertriglyceridemia in HIV-infected subjects on antiretroviral therapy: results of ACTG A5186. J Acquir Immune Defic Syndr. 2008;47:459-66.[PubMed Abstract] -
- Gingo MR, Morris A, Crothers K. Human immunodeficiency virus-associated obstructive lung diseases. Clin Chest Med. 2013;34:273-82.[PubMed Abstract] -
- Glesby MJ, Hoover DR, Shi Q, et al. Glycated haemoglobin in diabetic women with and without HIV infection: data from the Women's Interagency HIV Study. Antivir Ther. 2010;15:571-7.[PubMed Abstract] -
- Gomes AC, Aragüés JM, Guerra S, Fernandes J, Mascarenhas MR. Hypogonadotropic hypogonadism in human immunodeficiency virus-infected men: uncommonly low testosterone levels. Endocrinol Diabetes Metab Case Rep. 2017;2017:17-0104.[PubMed Abstract] -
- Gourlay ML, Fine JP, Preisser JS, et al. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-33.[PubMed Abstract] -
- Grinspoon S, Corcoran C, Askari H, et al. Effects of androgen administration in men with the AIDS wasting syndrome. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;129:18-26.[PubMed Abstract] -
- Grinspoon SK, Fitch KV, Overton ET, et al. Rationale and design of the Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE). Am Heart J. 2019;212:23-35.[PubMed Abstract] -
- Gupta SK, Eustace JA, Winston JA, et al. Guidelines for the management of chronic kidney disease in HIV-infected patients: recommendations of the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2005;40:1559-85.[PubMed Abstract] -
- Hajek P, Smith KM, Dhanji AR, McRobbie H. Is a combination of varenicline and nicotine patch more effective in helping smokers quit than varenicline alone? A randomised controlled trial. BMC Med. 2013;11:140.[PubMed Abstract] -
- Halpin DMG, Criner GJ, Papi A, et al. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2021;203:24-36.[PubMed Abstract] -
- Harris TG, Burk RD, Palefsky JM, et al. Incidence of cervical squamous intraepithelial lesions associated with HIV serostatus, CD4 cell counts, and human papillomavirus test results. JAMA. 2005;293:1471-6.[PubMed Abstract] -
- Helleberg M, Afzal S, Kronborg G, et al. Mortality attributable to smoking among HIV-1-infected individuals: a nationwide, population-based cohort study. Clin Infect Dis. 2012;56:727-34.[PubMed Abstract] -
- Hemmingsen B, Lund SS, Gluud C, et al. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;11:CD008143.[PubMed Abstract] -
- Heron JE, Bloch M, Vanguru V, Saunders J, Gracey DM. Renal proximal tubulopathy in an HIV-infected patient treated with tenofovir alafenamide and gentamicin: a case report. BMC Nephrol. 2020;21:339.[PubMed Abstract] -
- Hillman RJ, Berry-Lawhorn JM, Ong JJ, et al. International Anal Neoplasia Society Guidelines for the Practice of Digital Anal Rectal Examination. J Low Genit Tract Dis. 2019;23:138-46.[PubMed Abstract] -
- Hirani A, Cavallazzi R, Vasu T, et al. Prevalence of obstructive lung disease in HIV population: a cross sectional study. Respir Med. 2011;105:1655-61.[PubMed Abstract] -
- Ho T, Cusack RP, Chaudhary N, Satia I, Kurmi OP. Under- and over-diagnosis of COPD: a global perspective. Breathe (Sheff). 2019;15:24-35.[PubMed Abstract] -
- Hoffmann U, Lu MT, Olalere D, et al. Rationale and design of the Mechanistic Substudy of the Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE): Effects of pitavastatin on coronary artery disease and inflammatory biomarkers. Am Heart J. 2019;212:1-12.[PubMed Abstract] -
- Homa DM, Neff LJ, King BA, et al. Vital signs: disparities in nonsmokers' exposure to secondhand smoke--United States, 1999-2012. MMWR Morb Mortal Wkly Rep. 2015;64:103-8.[MMWR] -
- Jamal A, Agaku IT, O'Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults--United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2014;63:1108-12.[MMWR] -
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-20.[PubMed Abstract] -
- Jardine MJ, Ninomiya T, Perkovic V, et al. Aspirin is beneficial in hypertensive patients with chronic kidney disease: a post-hoc subgroup analysis of a randomized controlled trial. J Am Coll Cardiol. 2010;56:956-65.[PubMed Abstract] -
- KDIGO Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013; 3:1-150.
- Keller MJ, Burk RD, Xie X, et al. Risk of cervical precancer and cancer among HIV-infected women with normal cervical cytology and no evidence of oncogenic HPV infection. JAMA. 2012;308:362-9.[PubMed Abstract] -
- Khalsa A, Karim R, Mack WJ, et al. Correlates of prevalent hypertension in a large cohort of HIV-infected women: Women's Interagency HIV Study. AIDS. 2007;21:2539-41.[PubMed Abstract] -
- Kim PS, Woods C, Georgoff P, et al. A1C underestimates glycemia in HIV infection. Diabetes Care. 2009;32:1591-3.[PubMed Abstract] -
- Koegelenberg CF, Noor F, Bateman ED, et al. Efficacy of varenicline combined with nicotine replacement therapy vs varenicline alone for smoking cessation: a randomized clinical trial. JAMA. 2014;312:155-61.[PubMed Abstract] -
- Kooij KW, Wit FW, Bisschop PH, et al. Low bone mineral density in patients with well-suppressed HIV infection: association with body weight, smoking, and prior advanced HIV disease. J Infect Dis. 2014;211:539-48.[PubMed Abstract] -
- Kowalska JD, Reekie J, Mocroft A, et al. Long-term exposure to combination antiretroviral therapy and risk of death from specific causes: no evidence for any previously unidentified increased risk due to antiretroviral therapy. AIDS. 2012;26:315-23.[PubMed Abstract] -
- Krishnan N, Gittelsohn J, Ross A, et al. Qualitative Exploration of a Smoking Cessation Trial for People Living With HIV in South Africa. Nicotine Tob Res. 2018;20:1117-23.[PubMed Abstract] -
- Landray MJ, Haynes R, Hopewell JC, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371:203-12.[PubMed Abstract] -
- Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160:171.[PubMed Abstract] -
- Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844-57.[PubMed Abstract] -
- Lin JS, Piper MA, Perdue LA, et al. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;315:2576-94.[PubMed Abstract] -
- Lo J, Abbara S, Shturman L, et al. Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. AIDS. 2010;24:243-53.[PubMed Abstract] -
- Maki KC, Dicklin MR, Baum SJ. Statins and diabetes. Cardiol Clin. 2015;33:233-43.[PubMed Abstract] -
- Marcus JL, Chao C, Leyden WA, et al. Survival among HIV-infected and HIV-uninfected individuals with common non-AIDS-defining cancers. Cancer Epidemiol Biomarkers Prev. 2015;24:1167-73.[PubMed Abstract] -
- Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567-75.[PubMed Abstract] -
- Massad LS, Einstein MH, Huh WK, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet Gynecol. 2013;121:829-46.[PubMed Abstract] -
- Medina-Torne S, Ganesan A, Barahona I, Crum-Cianflone NF. Hypertension is common among HIV-infected persons, but not associated with HAART. J Int Assoc Physicians AIDS Care (Chic). 2011;11:20-5.[PubMed Abstract] -
- Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292-333.[PubMed Abstract] -
- Mills A, Crofoot G Jr, McDonald C, et al. Tenofovir Alafenamide Versus Tenofovir Disoproxil Fumarate in the First Protease Inhibitor-Based Single-Tablet Regimen for Initial HIV-1 Therapy: A Randomized Phase 2 Study. J Acquir Immune Defic Syndr. 2015;69:439-45.[PubMed Abstract] -
- Monroe AK, Dobs AS, Palella FJ, Kingsley LA, Witt MD, Brown TT. Morning free and total testosterone in HIV-infected men: implications for the assessment of hypogonadism. AIDS Res Ther. 2014;11:6.[PubMed Abstract] -
- Morgan DR, Malik PR, Romeo DP, Rex DK. Initial US evaluation of second-generation capsule colonoscopy for detecting colon polyps. BMJ Open Gastroenterol. 2016;3:e000089.[PubMed Abstract] -
- National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94-138.[PubMed Abstract] -
- Nudy M, Cooper J, Ghahramani M, Ruzieh M, Mandrola J, Foy AJ. Aspirin for Primary Atherosclerotic Cardiovascular Disease Prevention as Baseline Risk Increases: A Meta-Regression Analysis. Am J Med. 2020;133:1056-64.[PubMed Abstract] -
- Overton ET, Kitch D, Benson CA, et al. Effect of statin therapy in reducing the risk of serious non-AIDS-defining events and nonaccidental death. Clin Infect Dis. 2013;56:1471-9.[PubMed Abstract] -
- Perkins RB, Guido RS, Castle PE, et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J Low Genit Tract Dis. 2020;24:102-31.[PubMed Abstract] -
- Petrosky E, Bocchini JA Jr, Hariri S, et al. Use of 9-Valent Human Papillomavirus (HPV) Vaccine: Updated HPV Vaccination Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2015;64:300-4.[MMWR] -
- Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA. Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.[PubMed Abstract] -
- Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155:179-91.[PubMed Abstract] -
- Reddy KP, Kong CY, Hyle EP, et al. Lung Cancer Mortality Associated With Smoking and Smoking Cessation Among People Living With HIV in the United States. JAMA Intern Med. 2017;177:1613-1621.[PubMed Abstract] -
- Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104:739-50.[PubMed Abstract] -
- Robbins HA, Shiels MS, Pfeiffer RM, Engels EA. Epidemiologic contributions to recent cancer trends among HIV-infected people in the United States. AIDS. 2014;28:881-90.[PubMed Abstract] -
- Robertson DJ, Lee JK, Boland CR, et al. Recommendations on Fecal Immunochemical Testing to Screen for Colorectal Neoplasia: A Consensus Statement by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;152:1217-1237.e3.[PubMed Abstract] -
- Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am J Clin Pathol. 2012;137:516-42.[PubMed Abstract] -
- Sax PE, Zolopa A, Brar I, et al. Tenofovir alafenamide vs. tenofovir disoproxil fumarate in single tablet regimens for initial HIV-1 therapy: a randomized phase 2 study. J Acquir Immune Defic Syndr. 2014;67:52-8.[PubMed Abstract] -
- Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145-64.[PubMed Abstract] -
- Sigel K, Pitts R, Crothers K. Lung Malignancies in HIV Infection. Semin Respir Crit Care Med. 2016;37:267-76.[PubMed Abstract] -
- Singh D, Agusti A, Anzueto A, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53:pii: 1900164.[PubMed Abstract] -
- Sisson EM, Pamulapati L, Bucheit JD, Kelly MS, Dixon DL. Evolving Role of Non-Statin Therapy for the Management of Dyslipidemia and Cardiovascular Risk Reduction: Past, Present, and Future. Pharmacotherapy. 2018;38:164-171.[PubMed Abstract] -
- Siu AL. Screening for Abnormal Blood Glucose and Type 2 Diabetes Mellitus: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163:861-8.[PubMed Abstract] -
- Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164:279-96.[PubMed Abstract] -
- Stradling C, Chen YF, Russell T, Connock M, Thomas GN, Taheri S. The effects of dietary intervention on HIV dyslipidaemia: a systematic review and meta-analysis. PLoS One. 2012;7:e38121.[PubMed Abstract] -
- Subramanian S, Tawakol A, Burdo TH, et al. Arterial inflammation in patients with HIV. JAMA. 2012;308:379-86.[PubMed Abstract] -
- Sullivan J, Pravosud V, Mannino DM, Siegel K, Choate R, Sullivan T. National and State Estimates of COPD Morbidity and Mortality - United States, 2014-2015. Chronic Obstr Pulm Dis. 2018;5:324-33.[PubMed Abstract] -
- Thiébaut R, El-Sadr WM, Friis-Møller N, et al. Predictors of hypertension and changes of blood pressure in HIV-infected patients. Antivir Ther. 2005;10:811-23.[PubMed Abstract] -
- Tien PC, Schneider MF, Cox C, et al. Association of HIV infection with incident diabetes mellitus: impact of using hemoglobin A1C as a criterion for diabetes. J Acquir Immune Defic Syndr. 2012;61:334-40.[PubMed Abstract] -
- Tsai J, Homa DM, Gentzke AS, et al. Exposure to Secondhand Smoke Among Nonsmokers - United States, 1988-2014. MMWR Morb Mortal Wkly Rep. 2018;67:1342-1346.[PubMed Abstract] -
- U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2013 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute:2016.[CDC] -
- U.S. Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154:356-64.[PubMed Abstract] -
- United States Cancer Statistics. U.S. Cancer Statistics: Highlights from 2016 Incidence. U.S. Cancer Statistics Data Briefs, No. 8. June 2019[CDC] -
- US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564-75.[PubMed Abstract] -
- Venkatesan P. GOLD COPD report: 2023 update. Lancet Respir Med. 2023;11:18.[PubMed Abstract] -
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139-e596.[PubMed Abstract] -
- Wang TW, Asman K, Gentzke AS, et al. Tobacco Product Use Among Adults - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67:1225-1232.[PubMed Abstract] -
- Wender R, Fontham ET, Barrera E Jr, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63:107-17.[PubMed Abstract] -
- Womack JA, Goulet JL, Gibert C, et al. Increased risk of fragility fractures among HIV infected compared to uninfected male veterans. PLoS One. 2011;6:e17217.[PubMed Abstract] -
- Wright JT Jr, Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103-16.[PubMed Abstract] -
- Wunder DM, Bersinger NA, Fux CA, et al. Hypogonadism in HIV-1-infected men is common and does not resolve during antiretroviral therapy. Antivir Ther. 2007;12:261-5.[PubMed Abstract] -
- Zanni MV, Abbara S, Lo J, et al. Increased coronary atherosclerotic plaque vulnerability by coronary computed tomography angiography in HIV-infected men. AIDS. 2013;27:1263-72.[PubMed Abstract] -
Figures
 Figure 1 (Image Series). Cervical Cancer Screening Algorithms for People with HIV with a Cervix*See Opportunistic Infections Guidelines for HPV testing in persons aged 25-29 years
Figure 1 (Image Series). Cervical Cancer Screening Algorithms for People with HIV with a Cervix*See Opportunistic Infections Guidelines for HPV testing in persons aged 25-29 years
Abbreviations: ASC-US = atypical squamous cells of undetermined significance; LSIL: low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 1B. Persons Aged 30 Years and Older: hr-HPV Testing Performed^If at repeat testing either cytology is ≥ASC-US or any hr-HPV is detected, refer for colposcopy (AII)
Figure 1B. Persons Aged 30 Years and Older: hr-HPV Testing Performed^If at repeat testing either cytology is ≥ASC-US or any hr-HPV is detected, refer for colposcopy (AII)
Abbreviations: hr-HPV = high-risk human papillomavirus; ASC-US = atypical squamous cells of undetermined significance; LSIL: low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 1C. Persons Aged 30 Years and Older: hr-HPV Testing NOT PerformedAbbreviations: hr-HPV = high-risk human papillomavirus; ASC-US = atypical squamous cells of undetermined significance; LSIL: low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024.
Figure 1C. Persons Aged 30 Years and Older: hr-HPV Testing NOT PerformedAbbreviations: hr-HPV = high-risk human papillomavirus; ASC-US = atypical squamous cells of undetermined significance; LSIL: low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 2 (Image Series). Anal Cancer Screening Algorithms for People with HIV
Figure 2 (Image Series). Anal Cancer Screening Algorithms for People with HIV*No specimen collected
Abbreviation: DARE = digital anorectal examination; HPV = human papillomavirus; hr-HPV = high-risk HPV; LSIL = low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 2B. Assessment of Anal Cytology and HPV Results: hr-HPV Co-Testing NOT PerformedAbbreviation: hr-HPV = high-risk human papillomavirus; ASC-US = atypical squamous cells of undetermined significanceSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024.
Figure 2B. Assessment of Anal Cytology and HPV Results: hr-HPV Co-Testing NOT PerformedAbbreviation: hr-HPV = high-risk human papillomavirus; ASC-US = atypical squamous cells of undetermined significanceSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 2C. Assessment of Anal Cytology and HPV Results: hr-HPV Co-Testing Performed^If at repeat testing either cytology is ≥ASC-US or any hr-HPV is detected, refer for colposcopy (AII)
Figure 2C. Assessment of Anal Cytology and HPV Results: hr-HPV Co-Testing Performed^If at repeat testing either cytology is ≥ASC-US or any hr-HPV is detected, refer for colposcopy (AII)
Abbreviations: HPV = human papillomavirus; hr-HPV = high-risk HPV; ASC-US = atypical squamous cells of undetermined significance; LSIL = low-grade squamous intraepithelial lesionSource: Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Human papillomavirus disease. July 9, 2024. Figure 3. Summary of Three Aspirin Trials for Primary Prevention of Cardiovascular DiseaseSource: Knickelbine T, Miedema MD. Aspirin for primary prevention of cardiovascular disease: is it time to move on? Curr Opin Cardiol. 2019;34:510-13.
Figure 3. Summary of Three Aspirin Trials for Primary Prevention of Cardiovascular DiseaseSource: Knickelbine T, Miedema MD. Aspirin for primary prevention of cardiovascular disease: is it time to move on? Curr Opin Cardiol. 2019;34:510-13. Figure 4 (Image Series). Cardiovascular Risk in Persons with HIVSource: Klein D, Hurley LB, Quesenberry CP Jr, Sidney S. Do protease inhibitors increase the risk for coronary heart disease in patients with HIV-1 infection? J Acquir Immune Defic Syndr. 2002;30:471-7.
Figure 4 (Image Series). Cardiovascular Risk in Persons with HIVSource: Klein D, Hurley LB, Quesenberry CP Jr, Sidney S. Do protease inhibitors increase the risk for coronary heart disease in patients with HIV-1 infection? J Acquir Immune Defic Syndr. 2002;30:471-7. Figure 4B. Veterans Aging Cohort: Rates of Acute Myocardial Infarction by HIV Status and Age GroupSource: Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614-22.
Figure 4B. Veterans Aging Cohort: Rates of Acute Myocardial Infarction by HIV Status and Age GroupSource: Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614-22. Figure 5. Prevalence of Hypertension Among Adults 18 Years of Age and Older, by Gender and Age Group, NHANES, 2017-2018Source: National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey (NHANES). Fact Sheet. July 2020.
Figure 5. Prevalence of Hypertension Among Adults 18 Years of Age and Older, by Gender and Age Group, NHANES, 2017-2018Source: National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey (NHANES). Fact Sheet. July 2020. Figure 6. 2017 Hypertension Guidelines: Categories of Blood Pressure for AdultsSource: Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269.
Figure 6. 2017 Hypertension Guidelines: Categories of Blood Pressure for AdultsSource: Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269. Figure 7. American College of Cardiology-American Heart Association Cholesterol Guidelines: Intensity of StatinsSource: Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143.
Figure 7. American College of Cardiology-American Heart Association Cholesterol Guidelines: Intensity of StatinsSource: Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143. Figure 8. Impact of Antiretroviral Medications on Lipid LevelsSource: Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. Limitations to treatment safety and efficacy: adverse effects of antiretroviral agents. October 28, 2018.
Figure 8. Impact of Antiretroviral Medications on Lipid LevelsSource: Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. Limitations to treatment safety and efficacy: adverse effects of antiretroviral agents. October 28, 2018. Figure 9. GFR Categories in Chronic Kidney DiseaseSource: National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1-266.
Figure 9. GFR Categories in Chronic Kidney DiseaseSource: National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1-266. Figure 10. Prognosis of Chronic Kidney Disease by GFR and Albuminuria Categories: KIDGO 2012Abbreviations: GFR = glomerular filtration rateSource: Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713-35.
Figure 10. Prognosis of Chronic Kidney Disease by GFR and Albuminuria Categories: KIDGO 2012Abbreviations: GFR = glomerular filtration rateSource: Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713-35. Figure 11. Common Laboratory Indicators of Proximal Tubular DysfunctionSource: Lucas GM, Ross MJ, Stock PG, et al. Clinical Practice Guideline for the Management of Chronic Kidney Disease in Patients Infected With HIV: 2014 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96-e138.
Figure 11. Common Laboratory Indicators of Proximal Tubular DysfunctionSource: Lucas GM, Ross MJ, Stock PG, et al. Clinical Practice Guideline for the Management of Chronic Kidney Disease in Patients Infected With HIV: 2014 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96-e138. Figure 12. Effectiveness and Abstinence Rates for Various Medications at 6 Months after QuittingSource: U.S. Public Health Service. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158-76.
Figure 12. Effectiveness and Abstinence Rates for Various Medications at 6 Months after QuittingSource: U.S. Public Health Service. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158-76.Tables
Table 1. U.S. Multi-Society Task Force on Colorectal CancerMulti-Society Task Force Ranking of Current Colorectal Cancer Screening Tests
Tier 1
- Colonoscopy every 10 years
- Annual fecal immunochemical test (FIT)
Tier 2
- CT colonography every 5 years
- FIT-fecal DNA every 3 years
- Flexible sigmoidoscopy every 10 years (or every 5 years)
Tier 3 - Capsule colonoscopy every 5 years
Available Tests Not Currently Recommended
- Septin 9
Source:- Rex DK, Boland CR, Dominitz JA, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307-23. [PubMed Abstract]
Table 2. U.S. Multi-Society Task Force on Colorectal CancerUS Multi-Society Task Force Recommendations for Post-Colonoscopy Follow-Up in Average-Risk Adults With Normal Colonoscopy or Adenomasa
Baseline Colonoscopy:
Most Advanced Finding(s)Recommended Surveillance Interval Strength of Recommendation Quality of Evidence Normal 10 yearsb Strong High 1–2 tubular adenomas <10 mm 7-10 yearsc Strong Moderate 3-4 tubular adenomas <10 mm 3-5 years Weak Very low 5–10 tubular adenomas <10 mm 3 years Strong Moderate Adenoma >10 mm 3 years Strong High Adenoma with tubulovillous or villous histology 3 yearsd Strong Moderate Adenoma with high-grade dysplasia 3 yearsd Strong Moderate >10 adenomas on single examinatione 1 year Weak Very low Piecemeal resection of adenoma ≥20 mm 6 months Strong Moderatef aAll recommendations assume examination complete to cecum with bowel preparation adequate to detect lesions >5 mm in size; recommendations do not apply to individuals with a hereditary CRC syndrome, personal history of inflammatory bowel disease, personal history of hereditary cancer syndrome, serrated polyposis syndrome, malignant polyp, personal history of CRC, or family history of CRC, and must be judiciously applied to such individuals, favoring the shortest indicated interval based on either history or polyp findings.
bFollow-up may be with colonoscopy or other screening modality for average-risk individuals.
c Patients with recommendations issued before 2020 for shorter than 7- to 10-year follow-up after diagnosis of 1–2 tubular adenomas may follow original recommendations. If feasible, physicians may re-evaluate patients previously recommended an interval shorter than 10 y and reasonably choose to provide an updated recommendation for 7- to 10-year follow-up, taking into account factors such as quality of baseline examination, polyp history, and patient preferences.
dAssumes high confidence of complete resection.
ePatients with >10 adenomas or lifetime >10 cumulative adenomas may need to be considered for genetic testing based on absolute/cumulative adenoma number, patient age, and other factors such as family history of CRC (see text).
fSee US Multi-Society Task Force recommendations for endoscopic removal of colorectal lesions.
Source:- Gupta S, Lieberman D, Anderson JC, et al. Recommendations for Follow-Up After Colonoscopy and Polypectomy: A Consensus Update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2020;158:1131-53.e5. [PubMed Abstract]
Table 3. American Diabetes Association (ADA) Standards of Medical Care in Diabetes—2023Criteria for Testing for Diabetes or Prediabetes in Asymptomatic Adults
1. Testing should be considered in overweight or obese (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian Americans) adults who have one or more of the following risk factors:
- First-degree relative with diabetes
- Race/ethnicity with increased risk of developing diabetes (e.g., African American, Latino, Native American, Asian American, Pacific Islander)
- History of cardiovascular disease
- Hypertension (≥130/80 mmHg or on therapy for hypertension)
- HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L)
- Women with polycystic ovary syndrome
- Physical inactivity
- Other clinical conditions associated with insulin resistance (e.g., severe obesity, acanthosis nigricans)
2. Patients with prediabetes (HbA1c ≥5.7% [39 mmol/mol], impaired glucose tolerance, or impaired fasting glucose) should be tested yearly. 3. Women who were diagnosed with gestational diabetes mellitus should have lifelong testing at least every 3 years. 4. For all other patients, testing should begin at 35 years of age. 5. If results are normal, testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status. 6. People with HIV Source:- ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46:S19-S40. [PubMed Abstract]
Table 4. 2017 Hypertension Guidelines: Blood Pressure Targets and Treatment Recommendations
BP Category Systolic Diastolic Treatment or Follow-Up Normal <120 mm/Hg and <80 mm/Hg Evaluate yearly; encourage healthy lifestyle changes to maintain normal BP Elevated 120-129 mm/Hg and <80 mm/Hg Recommend healthy lifestyle changes and reassess in 3 to 6 months Hypertension: Stage 1 130-139 mm/Hg or 80-89 mm/Hg Assess the 10-year risk for heart disease and stroke using the atherosclerotic cardiovascular disease (ASCVD) risk calculator
- If risk is less than 10%, start with healthy lifestyle recommendations and reassess in 3 to 6 months
- If risk is greater than 10% or the patient has known clinical cardiovascular disease (CVD), diabetes mellitus, or chronic kidney disease, recommend lifestyle changes and BP-lowering medication (1 medication); reassess in 1 month for effectiveness of medication therapy
- If goal is met after 1 month, reassess in 3 to 6 months
- If goal is not met after 1 month, consider different medication or titration
- Continue monthly follow-up until control is achieved
Hypertension: Stage 2 ≥140 mm/Hg or ≥90 mm/Hg Recommend healthy lifestyle changes and BP-lowering medication (initiate with 2 medications of different classes); reassess in 1 month for effectiveness
- If goal is met after 1 month, reassess in 3 to 6 months
- If goal is not met after 1 month, consider different medications or titration
- Continue monthly follow-up until control is achieved
Source:- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199-2269. [PubMed Abstract]
Table 5. 2018 American College of Cardiology/American Heart Association Guideline on the Management of Blood CholesterolAtherosclerotic Cardiovascular Disease (ASCVD) Risk Enhancers
Clinical Factors • Family history of premature ASCVD • Persistent elevated LDL-C ≥160 mg/dL (≥4.1 mmol/L) • Chronic kidney disease • Metabolic syndrome • Conditions specific to women (e.g. preeclampsia, premature menopause) • Inflammatory Diseases (especially rheumatoid arthritis, psoriasis, HIV) • Ethnicity (e.g. South Asian ancestry) Lipid/Biomarkers • Persistently elevated triglycerides (≥175 mg/dL, [≥2.0 mmol/L]) Heterozygous familial hypercholesterolemia • Elevated high-sensitivity C-reactive Protein (CRP) ≥2.0 mg/L • Lipoprotein (a) levels ≥50 mg/dL (or ≥125 nmol/L) • apoB ≥130 mg/dL • Current smoking • Ankle-brachial index (ABI) <0.9 Abbreviations: ASCVD = atherosclerotic cardiovascular disease; LDL-C = low density lipoprotein cholesterol; hs-CRP = high sensitivity C-reactive protein Source:- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143. [PubMed Abstract]
Table 6. 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment.FDA-Approved Recommended Medications for Tobacco Cessation Treatment*
Drug
(doses)How Sold (U.S.) Dosing Instructions Administration Common Side Effects Advantages Disadvantages Nicotine patch
21 mg
14 mg
7 mgOTC or Rx Starting dose:
21 mg for ≥10 cigarettes per day.
14 mg for <10 cigarettes per day.
After 6 weeks, option to taper to lower doses for 2-6 weeks.
Use ≥3 months.
After 6 weeks, continue original dose or taper to lower doses (either option acceptable).Apply a new patch each morning to dry skin.
Rotate application site to avoid skin irritation.
May start patch before or on quit date.
Keep using even if a slip occurs.
If insomnia or disturbing dreams, remove patch at bedtime.Skin irritation
Trouble sleeping
Vivid dreams (patch can be removed at bedtime to manage insomnia or vivid dreams)
The easiest nicotine product to use.
Provides a steady nicotine level.
Combination NRT therapy: as needed, can add gum, lozenge, inhaler, or nasal spray to patch to cover situational cravings.User cannot alter dose if cravings occur during the day. Nicotine lozenge
4 mg
2 mgOTC or Rx If first cigarette is ≤30 minutes of waking: 4 mg.
If first cigarette is >30 minutes of waking: 2 mg.
Use ≥3 months.Place between gum and cheek, let it melt slowly.
Use 1 piece every 1-2 hours (Max: 20/day).Mouth irritation
Hiccups
Heartburn
NauseaUser controls nicotine dose.
Oral substitute for cigarettes.
May be added to patch to cover situational cravings.
Easier to use than gum for those with dental work or dentures.No food or drink 15 minutes prior to use and during use. Nicotine gum
4 mg
2 mg
OTC or Rx If first cigarette is ≤30 minutes of waking: 4 mg.
If first cigarette is >30 minutes of waking: 2 mg.
Use ≥3 months.Chew briefly until mouth tingles, then ‘park’ gum inside cheek until tingle fades. Repeat chew-and-park each time tingle fades. Discard gum after 30 minutes of use.
Use ~ 1 piece per hour (Max: 24/day).Mouth irritation
Jaw soreness
Heartburn
Hiccups
Nausea
User controls nicotine dose.
Oral substitute for cigarettes.
May be added to patch to cover situational cravings.
Not chewed in same way as regular gum; requires careful instruction.
Can damage dental work and be difficult to use with dentures.
No food or drink 15 minutes prior to use and during use.Nicotine inhaler
10-mg cartridgeRx only 10 mg/cartridge.
Each cartridge has ~80 puffs.
Use ≥3 months.Puff into mouth/throat until cravings subside. Do not inhale into lungs.
Change cartridge when nicotine taste disappears.
Use 1 cartridge every 1-2 hours (Max: 16/day).Mouth and throat irritation
Coughing if inhaled too deeplyUser controls nicotine dose.
Mimics hand-to-mouth ritual of smoking cigarettes.
May be added to patch to cover situational cravings.Frequent puffing required. Nicotine nasal spray
10 mg/mL
(10 mL bottle)Rx only 10 mg/mL.
0.5 mg per spray.
Each bottle has ~200 sprays.
Use ≥3 months.Use 1 spray to each nostril.
Use spray every 1-2 hours (Max: 80/day).Nasal and throat irritation
Rhinitis
Sneezing
Coughing
TearingUser controls nicotine dose.
Most rapid delivery of nicotine among all NRT products.
May be added to patch to cover situational cravings.Has the most side effects of all NRT products.
Some users cannot tolerate local irritation to nasal mucosa.Varenicline (tablet)
0.5 mg
1.0 mgRx only Days 1-3: 0.5 mg/day.
Days 4-7: 0.5 mg twice a day.
Day 8+: 1 mg twice a day.
Use 3-6 months.
Start 1-4 weeks before quit date.
Take with food and a tall glass of water to minimize nausea.Nausea
Insomnia
Vivid dreams
HeadacheQuit date can be flexible, from 1 week to 3 months after starting drug.
Dual action:relieves nicotine withdrawal and blocks reward of smoking.
Oral agent (pill).Because of previous FDA warning (now removed), many patients fear psychiatric adverse events, even though they are no more common than with other cessation medications. Bupropion sustained release (SR) (tablet)
150 mgRx only 150 mg/day for 3 days, then 150 mg twice a day.
Use 3-6 months.Start 1-2 weeks before quit date. Insomnia
Agitation
Dry mouth
HeadacheMay lessen post-cessation weight gain while drug is being taken.
Oral agent (pill).Increases seizure risk: not for use if seizure disorder or binge drinking. * All are FDA-approved as smoking cessation aids and listed as a first-line medication by U.S. Clinical Practice Guidelines (Fiore, 2008)
+ Recommended duration of use for medications is at least 3 months but extending dose to 6 months is frequently done to prevent relapse to tobacco use. Patching dosing differs slightly from FDA labeling.
Abbreviations: FDA = U.S. Food and Drug Administration; NRT = nicotine replacement therapy; OTC = over the counter (no prescription required); Rx = prescription required.
Source:- Barua RS, Rigotti NA, Benowitz NL, et al. 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2018;72:3332-65. [PubMed Abstract]
Share by e-mail
Check
-On-
Learning
QuestionsThe Check-on-Learning Questions are short and topic related. They are meant to help you stay on track throughout each lesson and check your understanding of key concepts.You must be signed in to customize your interaction with these questions.
Funded byHealth Resources and Services Administration (HRSA)Created at University of WashingtonAn AETC ProgramPart of IDEA PlatformCME provided byUniversity of Alabama BirminghamCNE provided byUniversity of Washington School of NursingCopyright © 2024 National HIV CurriculumThe National HIV Curriculum is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $1,172,990 with 0% financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.govSince you've received 80% or better on this quiz, you may claim continuing education credit.
You seem to have a popup blocker enabled. If you want to skip this dialog please Always allow popup windows for the online course.
Current Version: nhivc-master-6c628bd7-2024-12-09-232956 - 0%Lesson 2
 Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy
Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza
Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Dolutegravir-Abacavir-Lamivudine Triumeq
Dolutegravir-Abacavir-Lamivudine Triumeq Dolutegravir-Lamivudine Dovato
Dolutegravir-Lamivudine Dovato Dolutegravir-Rilpivirine Juluca
Dolutegravir-Rilpivirine Juluca Doravirine-Tenofovir DF-Lamivudine Delstrigo
Doravirine-Tenofovir DF-Lamivudine Delstrigo Efavirenz-Tenofovir DF-Emtricitabine Atripla
Efavirenz-Tenofovir DF-Emtricitabine Atripla Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya
Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild
Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey
Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey Rilpivirine-Tenofovir DF-Emtricitabine Complera
Rilpivirine-Tenofovir DF-Emtricitabine Complera Enfuvirtide Fuzeon
Enfuvirtide Fuzeon Fostemsavir Rukobia
Fostemsavir Rukobia Ibalizumab Trogarzo
Ibalizumab Trogarzo Maraviroc Selzentry
Maraviroc Selzentry Dolutegravir Tivicay
Dolutegravir Tivicay Raltegravir Isentress
Raltegravir Isentress Abacavir Ziagen
Abacavir Ziagen Abacavir-Lamivudine Epzicom
Abacavir-Lamivudine Epzicom Abacavir-Lamivudine-Zidovudine Trizivir
Abacavir-Lamivudine-Zidovudine Trizivir Didanosine Videx
Didanosine Videx Emtricitabine Emtriva
Emtricitabine Emtriva Lamivudine Epivir
Lamivudine Epivir Stavudine Zerit
Stavudine Zerit Tenofovir alafenamide-Emtricitabine Descovy
Tenofovir alafenamide-Emtricitabine Descovy Tenofovir DF Viread
Tenofovir DF Viread Tenofovir DF-Emtricitabine Truvada and Multiple Generics
Tenofovir DF-Emtricitabine Truvada and Multiple Generics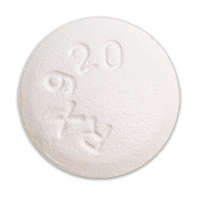 Zidovudine Retrovir
Zidovudine Retrovir Zidovudine-Lamivudine Combivir
Zidovudine-Lamivudine Combivir Doravirine Pifeltro
Doravirine Pifeltro Efavirenz Sustiva
Efavirenz Sustiva Etravirine Intelence
Etravirine Intelence Nevirapine Viramune
Nevirapine Viramune Rilpivirine Edurant
Rilpivirine Edurant Atazanavir Reyataz
Atazanavir Reyataz Atazanavir-Cobicistat Evotaz
Atazanavir-Cobicistat Evotaz Darunavir Prezista
Darunavir Prezista Darunavir-Cobicistat Prezcobix
Darunavir-Cobicistat Prezcobix Fosamprenavir Lexiva
Fosamprenavir Lexiva Indinavir Crixivan
Indinavir Crixivan Lopinavir-Ritonavir Kaletra
Lopinavir-Ritonavir Kaletra Nelfinavir Viracept
Nelfinavir Viracept Saquinavir Invirase
Saquinavir Invirase Tipranavir Aptivus
Tipranavir Aptivus Cobicistat Tybost
Cobicistat Tybost Ritonavir Norvir
Ritonavir Norvir















